Himmelfarb Health Sciences Library, The George Washington University Himmelfarb Health Sciences Library, The George Washington University
Health Sciences Research Commons Health Sciences Research Commons
Doctor of Nursing Practice Projects Nursing
Spring 2020
Using Five Wishes to Improve Advance Care Planning in A Using Five Wishes to Improve Advance Care Planning in A
Maryland Primary Care Practice Maryland Primary Care Practice
Amanda Bridges, MSN, ACNP-BC
George Washington University
Follow this and additional works at: https://hsrc.himmelfarb.gwu.edu/son_dnp
Part of the Nursing Commons
Recommended Citation Recommended Citation
Bridges, MSN, ACNP-BC, A. (2020). Using Five Wishes to Improve Advance Care Planning in A Maryland
Primary Care Practice.
,
(). Retrieved from https://hsrc.himmelfarb.gwu.edu/son_dnp/59
This DNP Project is brought to you for free and open access by the Nursing at Health Sciences Research
Commons. It has been accepted for inclusion in Doctor of Nursing Practice Projects by an authorized administrator
of Health Sciences Research Commons. For more information, please contact [email protected].

Running head: FIVE WISHES 1
Using Five Wishes to Improve Advance Care Planning in A Maryland Primary Care Practice
Amanda Bridges MSN, ACNP-BC
The George Washington University
March 21, 2020
DNP Primary Advisor: Richard Ricciardi, PhD, CRNP, FAANP, FAAN
DNP Second Advisor: Mary-Michael Brown, DNP, RN
FIVE WISHES 2
A Project Presented to the Faculty of the School of Nursing
The George Washington University
In partial fulfillment of the requirements
For the Degree of Doctor of Nursing Practice
By
Amanda Bridges, ACNP-BC
Approved: Richard Ricciardi, PhD
Approved: Mindi Cohen, DO
Approval Acknowledged:
Director DNP Scholarly Projects
Approval Acknowledged: Dr. Mercedes Echevarria
Assistant Dean for DNP Program
Date: April 4, 2020
Approved:
ary
Micha
Brown,
DNP
FIVE WISHES 3
Table of Contents
Cover Page.………………………………………………………………………………….....
1
Table of Content………………………………………………………………………………..
2
Abstract…………………………………………………………………………………………
5
Introduction……………………………………………………………………………………..
7
Background and Significance…………………………………………………………………..
8
Needs Assessment……………………………………………………………………………....
11
Problem Statement……………………………………………………………………………...
14
Aims and Objectives……………………………………………………………………………
14
Review of the Literature………………………………………………………………………..
15
Evidence Based Practice Model………………………………………………………………..
18
Methodology…………………………………………………………………………………....
19
Setting……………………………………………………………………………………
Study Population………………………………………………………………………....
Subject Recruitment……………………………………………………………………...
Consent Procedure……………………………………………………………………….
Risks/Harms……………………………………………………………………………...
Subject Costs and Compensation………………………………………………………...
Study Interventions………………………………………………………………………
Outcomes to be Measured………………………………………………………………..
Project Timeline………………………………………………………………………….
Resources Needed…………………………………………………………………….….
21
21
22
22
23
23
24
25
26
27
FIVE WISHES 4
Results……….…………………………………………………………………………………
27
Discussion……………………………………………………………………………………...
30
Sustainability and Future Scholarship………………………………………………………….
32
Conclusion…..……………………………………………………………………………….…
32
References……………………………………………………………………………………...
36
Appendices….………………………………………………………………………………….
40
Literature Review…….….……………………………………………………………….
Five Wishes Questionnaire……………………………………………………………….
Five Wishes Consent……..……………………………………………………………….
Shared Decision Making Tool…..…….………………………………………………….
40
52
53
54
Kiosk ACP Questions for EHR.…………………………………………………………..
Five Wishes Invitational Flyer……..….………………………………………………….
Data Definitions/Demographics………..…………………………………………………
IRB Documents…………………………..……………………………………………….
DNP Team Signature Sheet………………......…………………………………………..
55
56
57
66
68
FIVE WISHES 5
Tables and Figures
Table 1
Cost and Benefit Analysis……………………………………………….
58
Table 2
Evaluation….…………………………………………………………….
58
Table 3
Table 4
Table 5
Data Analysis…………………………………………………………….
Data Definitions………………………………………………………….
Variable Analysis Table………………………………………………….
60
63
63
Figure 1
Revised Johns Hopkins Model…………….…………………………….
33
Figure 2
Methodology Map….…………………………………………………….
34
Figure 3
Project Timeline...……………………………………………………….
35
FIVE WISHES 6
Abstract
Background
Engagement in Advance Care Planning (ACP) at this primary care practice is minimal with no consistent
process to document existing advance directives (AD) or educate about ADs.
Objectives
The purpose of this QI project was to increase ACP discussions, improve documentation of existing ADs and
educate about Five Wishes.
Methodology
Adults, at each office encounter, were asked three kiosk questions: Do you have an AD, know what it is and
want to discuss ACP? The responses were uploaded to the EHR to become an evidence backed, visual
reminder. Affirmation of existing ADs were descriptively documented. ACP engagement was analyzed by
chi square comparing responses to the questions and provider engagement in ACP. Everyone was invited to
a Five Wishes seminar and given the same questionnaire pre and post with mean responses assessed via a
paired t-test.
Results
The 1037 participants were mostly, employed, white, married and averaged age 52. After 12 weeks, 90 ACP
discussions took place compared to 6 discussions prior to implementation (p<0.001). At the seminar, 21
people had mean result with mixed statistically significance. The questions regarding value of Five Wishes
and discussing ACP were statistically significant (p<0.05). The total number of existing ADs was 23% of
1037 encounters.
FIVE WISHES 7
Conclusion
Engagement in ACP discussions improved by both asking about interest and creating EHR reminders. The
kiosk-initiated process makes this project sustainable and normalize ACP discussions. Five Wishes does not
meet legal requirements for an AD in every state and future policy should focus on full legalization.
FIVE WISHES 8
Using Five Wishes to Improve Advance Care Planning in a Maryland Primary Care Practice
An advance directive (AD) is a legal document intended to assist loved ones and medical
providers with end of life wishes when a person is unable to state their dying preferences for
medical care. In the state of Maryland, there are two forms that meet the legal requirements for
an AD: (a) Maryland Advance Directive: Planning for Future Health Care Decisions and (b) Five
Wishes (Advance Directive, n.d). The Maryland AD outlines both the designated person to
make medical decisions as well as several back up designations. Comfort and medical treatment
options are also covered along with the designation of organ donation and funeral arrangements
(Maryland Attorney General, n.d.).
Five Wishes is an AD that was developed by the nonprofit organization, Aging with
Dignity, and supported by a grant from the Robert Wood Johnson Foundation (Aging with
Dignity, 2012). This AD addresses the legal questions of health care power of attorney and
medical care desires for end of life care but also includes questions to address spirituality,
comfort, forgiveness and final wishes (Aging with Dignity, 2012). The five “wishes” are:
1. The person I want to make care decisions for me when I can’t
2. The kind of medical treatment I want
3. How comfortable I want to be
4. How I want people to treat me
5. What I want my loved ones to know
This project focused on improving advance care planning in a primary care practice with Five
Wishes.
FIVE WISHES 9
The process of completing an AD is often done in conjunction with a medical provider.
It is expected that a patient’s provider can guide decisions and answer questions about ACP.
ACP involves completing a chosen AD that is legally recognized by the state of residency. ADs
are instrumental in communicating patients’ wishes regarding end of life care and prevents loved
ones from the burden of making big medical decisions on someone else’s behalf. In addition,
ACP can improve the quality of end of life care and substantial decrease unnecessary hospital
admissions. However, the medical community, especially primary care, is vital to facilitating the
completion of this important document and thus efforts are needed to proactively engage primary
care providers and patients in having ACP discussions.
Background and Significance
The requirement for healthcare providers to facilitate ACP was established by the 1991
Patient Self-Determination Act (PDSA) which requires that any healthcare facility that receives
federal funding should discuss, educate, and facilitate the implementation of ADs (Douglas &
Brown, 2002). This established ADs as a standard of care. Recent advancements in healthcare
policy to further legislate AD use has had limited success. In 2009, the Affordable Care Act
(ACA) and the Advanced Planning and Compassionate Care Act both included efforts to
improve AD implementation by reimbursing physicians for ACP (Whelan, 2013).
Unfortunately, the factual content of the policy and myths surrounding potential “death panels”
resulted in removal of this aspect from the ACA (Whelan, 2013).
By the year 2030, all the baby boomers will have reached the age of 65 or older (Van
Wert, 2018), which will further increase the demand for an aging community to need ACP. This
places more pressure on primary care to develop a systematic process to facilitate ACP
discussions. To address this concern, Medicare ruled in November 2015 that ACP could be
FIVE WISHES 10
billed by providers as a Current Procedure Terminology (CPT) code for up to 30 minutes of
discussion starting January 1, 2016 (Verhovshek, 2016). Reimbursement for the first 30 minutes
of ACP equates to approximately $75 and an additional $70 for each additional 30 minutes
(Verhovshek, 2016). This reimbursement does not require the completion of an AD and can be
billed by any qualifying provider at each encounter where ACP is discussed, regardless of the
number of discussions (Verhhovshek, 2016). This was intended to create an incentive for
providers to improve ACP discussions, but financial incentives alone have not changed the
medical culture of discussion ACP.
According to a retrospective review of Medicare ACP billing in New England, less than
1% of the 2016 Medicare claims involved ACP (Pelland, Morphis, Harris & Gardner, 2019).
Providers are either not taking advantage of the reimbursement potential or have not effectively
created a process to discuss ACP in their medical practice. Likely, both reasons explain the lack
of implementation.
According to a 2014 “end of life” care survey, patients over the age of 18 years old were
surveyed regarding perception of end of life needs, discussions with loved ones about their end
of life desires, and existing advance directives (Rao, Anderson, Lin & Laux, 2014). Not
surprisingly, those of advanced age and with terminal diseases were more likely to have an AD.
Those who did not feel they had any end of life concern were less likely to complete an AD but
most of the participants surveyed lacked AD awareness (Rao, Anderson, Lin & Laux, 2014).
This lack of awareness highlights the need for primary care to proactively address AD education
in all patients before they become terminally ill or of advanced aged.
Advance care planning research to support AD use varies in design and often cannot
directly address the variable of cost due to ethical concerns. However, in 2018, Bond and
FIVE WISHES 11
colleagues (2018) evaluated ACP, retrospectively, in an Accountable Care Organization (ACO)
by comparing two groups of Medicare patients: those who had an AD at death versus those who
did not have an AD at death (Bond et. al., 2018). The authors reported that the AD group had a
nearly $10,000 adjusted savings compared to the control group (Bond et al., 2018). The authors
surmised that most of the cost savings to Medicare was in the reduction of inpatient admissions
(Bond et al., 2018). Saving money is not the main goal of any end of life discussion but reducing
unnecessary hospital admissions is a valuable goal. The discussion of ACP in terms of cost
savings is really a discussion about unnecessary hospital admissions.
There are three common reasons why people do not complete an AD: patients either
assume their loved ones know what they want, the patients do not understand ADs, or they fear
an AD will withhold medical care (Splendore & Grant, 2017). In general, the people who are
most likely to have an AD, are those with a terminal illness, of non-Hispanic, white race and
those of a higher socioeconomic status (Rao et al., 2014). According to the 2003 report on health
literacy from the US Department of Health and Human Resources, less than 13% of adults are
“proficient in understanding basic health information” with an even higher percentage of
Hispanic and elderly with even lower levels of literacy (n.d). The issue of health literacy
highlights the need for an ACP process in primary care that is repetitive, includes everyone and
has adjunctive educational options.
Shared decision making (SDM) is a core concern for this project. In order to improve
provider engagement in ACP, it is necessary for providers to have strong shared decision-making
skills. In a 2019 randomized control trial on the benefits of shared decision-making tools and
lung cancer screening, a subset of the LSUT (Lung Screening Uptake Trail) were assigned to two
methods of education on lung cancer screening. One group received the booklet alone and the
FIVE WISHES 12
other group received both the booklet and a video with a provider giving the education. In the
end, both groups had better understanding of lung cancer screening but the video group, showed
an even greater understanding (Ruparel, et.al, 2019). This highlights the value of various
mediums to address SDM with patients. This project addressed SDM with the provider via a
SDM educational brochure and a brief SDM oral presentation.
These factors are the historical aspects of ACP that were considered for this ACP
project. To successfully educate patients and reduce misconceptions, providers must be capable
of successful engagement in SDM. The information on ACP must be explained to patients via
various methods. Because reimbursement alone is not enough to encourage providers to have
ACP discussions, a simple, systems process is needed. Lastly, repeated opportunities for patients
to discuss ACP will facilitate normalization of ACP in primary care.
Needs Assessment
The previous process of addressing ACP at this project’s primary care practice, was done
inconsistently, by only a few providers during a Medicare annual wellness visit. Even when
patients had an AD, there was no consistent process to designate that an AD existed. In a review
of ACP discussions and CPT billing of ACP in Medicare patients for 2018, only 23 out of
approximately 3,000 enrolled Medicare patients had CPT billing for ACP in the 2018 calendar
year, for the entire practice (ECW, 2019). This primary care practice has office locations in
Maryland, Virginia and the District of Columbia. The wide geographical variability required
that this project start at one location in Maryland, over 12-weeks with future expectations to
implement this ACP project practice wide.
FIVE WISHES 13
A Strengths- Weakness-Opportunities-Threats (SWOT) analysis was done to evaluate the
feasibility of this ACP project. Strengths and opportunities for this project are substantial. The
strengths include an abundance of owner support for improving ACP. Employees are skillful
and cooperative and lastly, there is a practice wide EHR, which allows for data mining and
systematic processing. Additional strengths include three information technology (IT) support
staff who have various levels of IT responsibilities; one IT staff is a nurse practitioner. This
nurse practitioner assisted with data mining.
Weaknesses to this project include geographical distances between offices as some staff
who are instrumental to this project are located at other offices and communicate mainly via
email and phone. This distance did impede efficient and timely communication. Much of the
success of this project required both provider and ancillary staff “buy in” to ensure practice
change. The providers ability to successfully participate in SDM was not as significant a
weakness as expected. Medical assistant “buy in” was the most substantial weakness to this
project’s success. The ability of patients to use technology, like an electronic kiosk, was a
weakness. Given the Five Wishes educational seminars was provided only in English, there
were limited opportunities to educate non-English speaking patients about this specific AD.
However, copies of Five Wishes were available in two other languages, Russian and Spanish, for
providers and staff who speak the patient’s native language.
Opportunities for this project included continued practice growth through recent
acquisition of additional practice locations in Maryland and an alignment with a larger hospital
healthcare system to improve community resources. Given the expected volume of the aging
baby boomers, this project could model a successful ACP process for other primary care
practices to implement.
FIVE WISHES 14
The greatest threat to this project was the stigma of discussing death. Not surprisingly,
most patients did not want to discuss ACP. In general, Americans are often in denial about
death and do not plan for dying (Life in the USA, n.d). This is likely hindered by poor media
portrayal of dying and prior political influences on the topic of ACP.
There was a total of three providers, two physicians and one nurse practitioner, who
participated in this project at the Maryland location. The nurse practitioner works at this practice
location four days per week. Both physicians are the practice owners and see patients at other
office locations. These two physicians work at this location, one to two days per week. The
project utilized the front desk secretary and three medical assistants who disseminated
information and documented data in the EHR. Apart from one medical assistant and the front
desk secretary, all the other medical assistants rotate to other office locations throughout the
week. Having rotating staff members exposed to this QI project facilitates the opportunity to
implement this project at other offices. These staff members can become future super trainers
for other offices.
The practice’s strategic plan is to provide comprehensive care to all patients with a
substantial focus on care coordination for the vulnerable and Medicare population. No previous
attempts to implement a formal ACP program has been tried at this practice. This ACP QI
project upholds the paradigm of comprehensive care and service to the aging population by
improving holistic medical management.
Problem Statement
The problems addressed by this project were provider engagement in ACP,
documentation of existing ADs, and educating patients about an alternative AD known as Five

FIVE WISHES 15
Wishes. To increase ACP discussions, a process was needed to engage all patients and
encourage providers to initiate an ACP discussions. In general, most patients were not interested
in ACP. However, this was not assumed based on age or medical history and thus everyone was
asked about interest in discussing ACP, at each office encounter. The benefit of asking everyone
at every encounter was to improve patients’ familiarity with the topic. Familiarity with the topic
of ACP could result in the now 18-year-old understanding the importance of ACP when older
and chronic disease develops. Patient responses to the question about existing AD resulted in
consistent documentation in the EHR. Lastly, this project was supplemented with the additional
measure of an educational seminar, open to everyone, to learn more about a unique AD called
Five Wishes.
Aims and Objectives
The aims and objectives for this project were as follows. The first aim was to increase
provider engagement in ACP. The first aim was assessed objectively by the total number of
encounters that documented a discussion of ACP by ICD-10 code at the end of the 12- week
project compared to both the number of providers who engaged in ACP discussion in the 12-
weeks prior to the project and patient responses to interest in ACP. The second aim was to
create a process to document existing ADs. This was assessed by percentage of existing ADs
noted in the EHR over 12-weeks. The third aim was to provide a seminar that successfully
educated patients about the value of ACP and an alternative AD, known as Five Wishes.
Education of Five Wishes was evaluated by patient responses to a Likert scaled questionnaire
given pre and post seminar at each weekly session over 12-weeks. Each patient answered the
same questionnaire pre and post seminar (Appendix B) to assess their before and after perceived

FIVE WISHES 16
value of ACP and Five Wishes, specifically. The questionnaire was adapted from previous,
similar research on the educational value of a Five Wishes seminar (Hinderer, 2014).
Review of Literature
A literature review took place between February to June of 2019 (Appendix A). Using
the CINAHL database, research was evaluated using the search terms “advance care planning,”
and “end of life care” and the inclusion criteria of all adults, academic journals and research that
was less than 5-year-old. This resulted in 54 articles for evaluation. Articles that focused on a
specific subpopulation or in an inpatient setting were excluded. Ultimately, five articles of the
54 were accepted both as relevant to outpatient ACP and of acceptable quality. Another separate
CINAHL search was conducted specifically using the terms “Five Wishes” including only
adults, and academic journals in the past five years. This resulted in only three articles. One
article was excluded based on its focus on a specific subset of seriously ill patients. The two
remaining articles were similar educational seminars to this research design and thus used as
examples to establish the Five Wishes educational seminar.
Lastly, CINAHL was used again to search the terms “shared decision making”, “and”,
“tools or instruments”, “physicians or doctors”. This search excluded research outside of the
United States and included adults, academic journals, English language with an extension to
eight years (2011- 2019). This resulted in 18 articles. The extension beyond the standard five
years was needed to capture a simple, evidence-based tool that addressed SDM in providers.
The articles were all reviewed for both content and quality, with the most applicable to primary
care and of the best quality used for this analysis.
A resource librarian was consulted for assistance with obtaining permission to use the
Advance Directive Attitude Survey (ADAS). The attempt to use ADAS was unsuccessful.
FIVE WISHES 17
Excerpts of ADAS were publicly available and noted in various articles and complied to create
the Five Wishes questionnaire.
The quality of the articles was assessed using the Johns Hopkins Nursing Evidence Based
Practice Model and Guidelines (Dearholt & Dang, 2018). The articles’ assessed quality is noted
in Appendix A. This assessment tool qualifies research based on a scale from I-V with
subdivided criteria of a, b and c signally high, good and low quality. Level I research is
strongest and defined as a randomized control trials with level V representing experiential and
non-evidence-based data (Dearholt & Dang, 2018).
The evidence from the following articles supported the methodology to address the aim
of improving provider engagement in ACP discussions. First, providers must have the ability to
engage in SDM to improve ACP. Jensen and associates (2011) supported the value of SDM by
studying the effects of training physicians on the Four Habits of Communication (Appendix D)
versus no training. These authors noted that, even with minimal training, patients’ perceptions of
SDM improved for providers who had some communication training. Although an older article,
this article was included to highlight the value of, even minimal training, to improve providers’
SDM ability (2011). Forcino and others (2017) provided a valid tool to assess patient’s
perceptions of a provider’s ability to engage in SDM. The CollabRATE shared decision-making
tool is a short three question tool with validity in numerous geographical primary care settings
(Forcino, et. al., 2017). This tool did not fit into my methodology but highlights the value of
SDM. Hayek and associates (2014) indicated that a provider’s ability to successfully engage in
shared decision making with patients is a vital aspect to ACP discussions.
Next, a team approach with EHR reminders lends itself to more successful ACP and
satisfaction with end of life care. Reinhardt and associates described a team approach to
FIVE WISHES 18
discussing end of life care and its positive impact on the loved ones who managed a patient’s end
of life wishes. Reinhardt et al. (2014) highlighted how ongoing conversations and ongoing
discussions improved AD documentation and ultimately, family members felt better about their
loved ones end of life care when an AD was in place (2014). Hayek and colleagues (2014)
offered strong evidence that provider reminders, especially in an EHR, were more successful in
improving AD implementation compared to no reminders. These authors concluded a direct
association between the number of reminders and number of AD completed (2013
The aim of improving education about Five Wishes was evaluated through research
results specifically about Five Wishes Educational Workshops. The articles that evaluated Five
Wishes education did not have a direct impact on the number of ADs implemented, however, all
articles validated the value to patient education. Hinderer & Lee (2014) and Splendore & Grant
(2017) developed educational programs to teach community adults about Five Wishes. Both
programs used community workshops to deliver the education. Neither program was associated
with a specific primary care practice. Both articles used a variation of a well-validated
questionnaire called the Advance Directive Attitude Survey (ADAS) to evaluate their
programs. As previously noted, attempts to obtain permission to use the full ADAS tool were
unsuccessful. Select questions from ADAS were reported in the article and used to create the
questionnaire for this project. Splendore & Grant’s Five Wishes educational seminar did report
an improvement in the patients’ perceived importance of ACP (2017). This article was
sponsored by the creators of Five Wishes. Hinderer & Lee (2014) used a community outreach
project to educated adults about Five Wishes. The sampling of people in this study did not
change their attitude about ACP but did statistically confirm that the educational program was
perceived as valuable to the participants based on the ADAS tool. This highlights that it takes
FIVE WISHES 19
more than just education to successfully implement an ACP program in clinical practice
(Hinderer, & Lee, 2014).
Evidence-based Practice (EBP) Translation Model
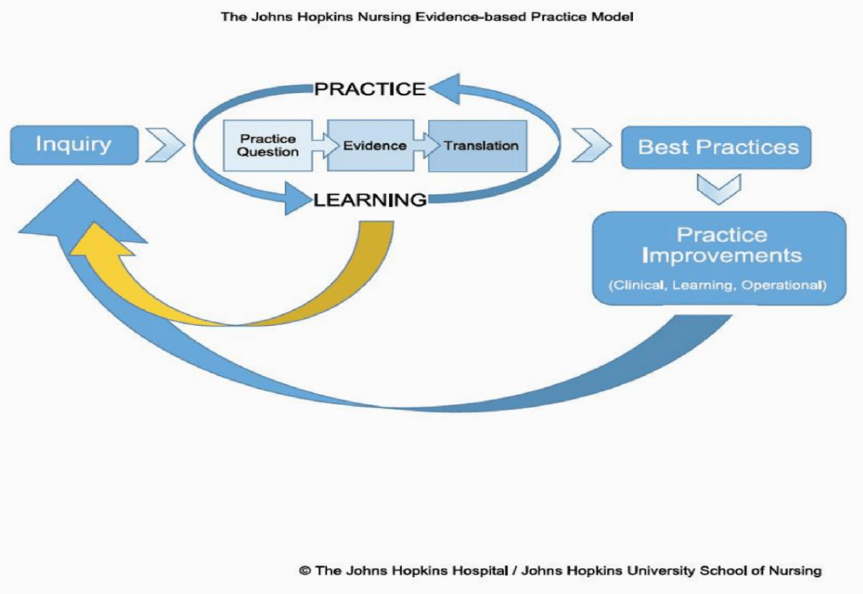
The revised Johns Hopkins Model (JHM) (Figure 1) was used as the evidence-based
translation model (Dearholt & Dang, 2018). This model was chosen for its inclusion of both
internal and external factors to influence best practices. This is especially important in ACP
where multiple internal and external factors impact implementation. An example of internal
factors includes a providers’ SDM ability to discuss ACP and an external factor is our societal
paradigms about death and dying. The process starts with an inquiry into the problem, followed
by the Practice, Evidence and Translation (PET) process to assess the question, gather the
evidence and translate the information into practice, all while learning new knowledge (Dearholt
& Dang, 2018).
The initial process of inquire started with identifying the need for ACP by assessing the
number of patients in the practice who have a documented discussion with their provider about
ACP. Next, practice owners’ interest in improving ACP was determined. Together, sufficiency
information supported the value of this project. This was then followed by gathering research
that was evaluated for quality, as mentioned, via Johns Hopkins Evidence Based Research
assessment. The research supported the value of improving shared decision making in
providers. Evidence also guided the internal and external influences on ACP. This information
was used to mitigate some of the research-based obstacles to implementing a ACP
process. Based on this information, a process was developed that teaches providers about
shared decision making and a systemic clinical process was developed to improve providers’
opportunities to discuss ACP with patients and document existing ADs. In addition, the
FIVE WISHES 20
research on other Five Wishes educational programs was modeled to address patient education
about this specific AD. During implementation, the internal and external influences guided the
teaching aspects that promote or inhibit implementation of ACP discussions, so practice change
can be successful.
Methodology
This is a quality improvement project that improved provider participation in ACP
discussions, documentation of existing ADs and education about the specific AD known as Five
Wishes. The evidence from prior research was incorporated into the methodology. The process
started with educating providers on shared decision making (SDM). Each provider was asked to
read an educational paper on how to improve their SDM ability (Appendix D). A short power
point presentation of SDM was given to all providers in the practice at our practice meeting prior
to implementation. Providers’ compliance with reading this educational paper on SDM was self-
reported. Patient recruitment to participate in ACP was through convenience sampling of those
who had an appointment at the Maryland office during the study implementation time
frame. Upon arriving at the appointment, all patients were asked three screening questions
about interest in discussing ACP via an electronic tablet enabled kiosk which was then uploaded
to the EHR by the medical assistant (Appendix E). A paper invitation to attend the informational
seminar on Five Wishes was given to every patient by the secretary (Appendix F). In addition, a
large electronic poster advertising the Five Wishes Seminar was on display in every exam room.
This electronic poster had the same information about the Five Wishes program date, time and
content (Appendix F). In addition, providers were asked to encourage all patients and their
family members to attend the Five Wishes seminar. Anyone could attend the Five Wishes
Seminar. After informed consent and a pre-seminar questionnaire, a 30-minute video created by
FIVE WISHES 21
Aging with Dignity was shown and followed by an informal question/answer session with an
eacute care nurse practitioner. The participants then completed the same questionnaire post
seminar. The questionnaire responses were via Likert scale that corresponded with perceived
value of both Five Wishes and ACP.
The following concepts noted in prior research were used in implementation. First,
shared decision making (SDM) was addressed with a short educational flyer and power point
presentation. Next, EHR documentation of patients who affirmed an existing AD was
consistently noted. Then, the patients’ responses to interest in an ACP discussion were uploaded
directly to the encounter note, in the EHR, creating an evidence backed, visual reminder
(Appendix E). If an ACP discussion was not possible during that office visit, patients were
asked to schedule another appointment to specifically discuss ACP or attend the educational
seminar on Five Wishes.
This project started on September 3, 2019 at a Maryland office location and ended
November 22, 2019. All data was mined through the EHR known as E-Clinical Works (ECW)
with the seminar evaluated by paper questionnaire responses (Appendix B). The Five Wishes
seminar was modeled after similar educational seminars noted in the literature review and a
similar questionnaire developed based on published exert of the ADAS questionnaire (Appendix
B). As noted, permission to use the ADAS tool was unsuccessful, but elements of this tool were
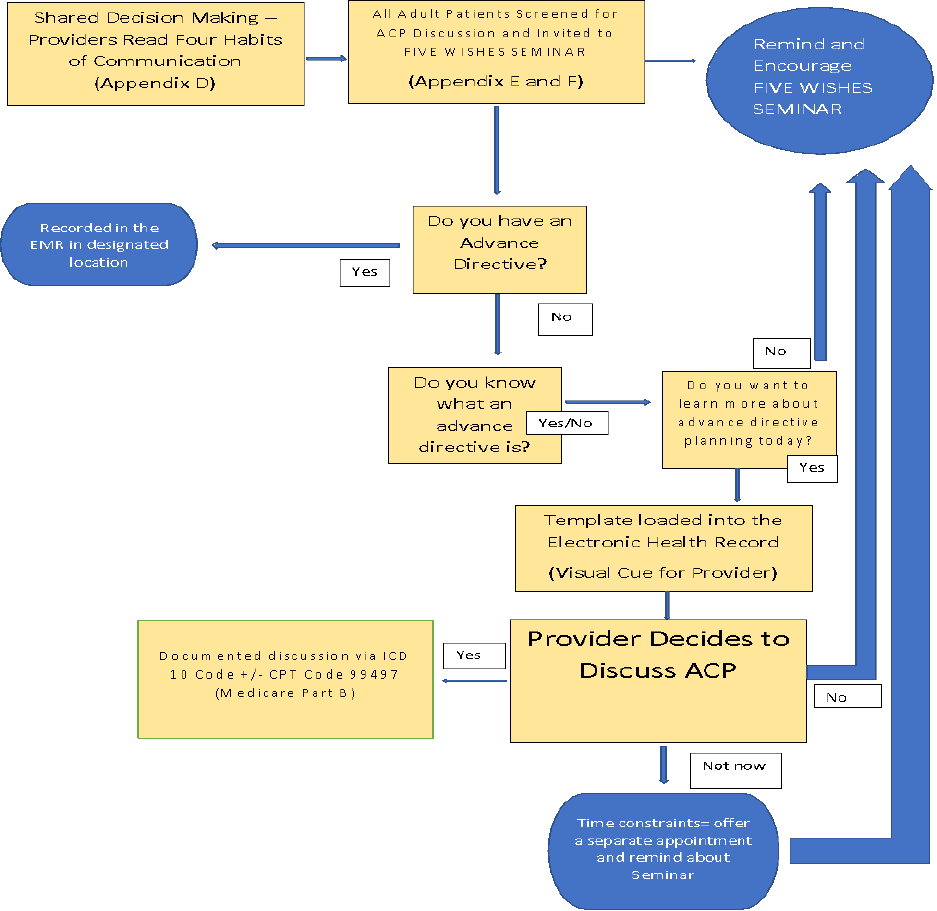
available in the literature review and used in creating the questionnaire (Appendix B). Figure 2
summarizes the project implementation process.
Setting
The setting for this QI project is a primary care practice in Maryland. The location of this
practice is in one of the highest educated cities in the United States and is situated just outside
FIVE WISHES 22
the nation’s capital, Washington, DC (Raghaven, D., 2014). The building for this practice
location typically accommodates only two providers and averages approximately 20 patient
encounters per day. The office location provides free parking and is conveniently located near
public transportation. The building is handicap accessible.
Study Population
There were two study groups evaluated. The first group consisted of a convenience
sampling of patients who met inclusion criteria and were seen at this office location between
September 2019 until November 2019. The second group were patients, loved ones and friends
who voluntarily attended the Five Wishes seminar during the implementation period. Inclusion
criteria for both groups were adults, defined as over the age of 18-year-old, of any race, gender,
or socioeconomic status. Patients who were blind or diagnosed with advanced dementia without
a designated power of attorney were excluded. All patients, family and friends were invited to
attend a free, weekly educational seminar on the AD known as Five Wishes. It was estimated
that approximately 1,200 patients would be offered ACP and invited to the Five Wishes Seminar
during the study period.
Patients who were seen at this location were mostly native English speaking, non-
Hispanic whites, however Russian and Spanish speaking patients are also seen at this
location. The Russian and Spanish speaking patients had varying fluency in English. Most non-
English speaking patients were seen by a provider who speaks their native language, or a native
speaking medical assistant translated for the provider. Most patients who received care at this
location, had a college education and were from a higher socioeconomic background. Patients
with a disability, had the same accommodations routinely provided.
FIVE WISHES 23
Subject Recruitment
Subject recruitment was via convenience sampling. All patients who met inclusion
criteria and were scheduled to see a provider during the study implementation period were
offered an opportunity to discuss ACP with their provider and given an invitational flyer on the
Five Wishes seminar (Appendix F). Participants in the Five Wishes workshop comprised of a
sampling from these patients, their family and friends. Electronic exam room posters
advertising the Five Wishes Seminar and were visible in all four examine rooms. The free
seminar took place on Thursday evenings from 5:00 to 6:30pm, each week, during the 12-week
study period. One seminar was cancelled due to AV equipment malfunctioning.
Consent Procedure
Consent to participate in the Five Wishes seminar was obtained in writing from the
patient by the nurse practitioner prior to each educational session (Appendix C). The patient
population seen for ACP engagement at the office location, did not require consent as assessing
interest in ACP is currently mandated by the 1991 PDSA and is a standard of care. In addition,
all patients have HIPPA protection of their personal health information (PHI). Discussions
about ACP in the office group was done privately between the provider and patient at the office
encounter in a closed, exam room. No PHI from either group was published. The paper
consents from the seminar were locked up in a secure cabinet inside the primary care practice
and will be destroyed in May 15, 2020.
Risks/Harms
There were minimal expected risks or harms associated with participation in ACP and the
Five Wishes seminars. Theoretically, a discussion about death could be emotionally upsetting
FIVE WISHES 24
for some patients. However, interest in discussing ACP with the patient’s provider was optional
and consistent with the standard of care. No patients were required to complete an AD nor
discuss ACP against their will.
Subject Costs/Compensation
A cost/benefit analysis is noted in Table 1. The cost of utilities, rent, and other
operational cost were minimal and already part of the practice’s current budget. The
implementation of this project required minimal, extra work from the current medical assistants
and the providers. Providers continued to be paid according to their contracts, which is based on
productivity, not hourly wages. The educational seminar took place in the office, after hours
when the office was traditionally vacant. No significant, extra cost was incurred from using the
building after hours. Although the seminar was led, voluntarily, by a nurse practitioner during
unpaid hours, for future consideration, the cost of a nurse led seminar has been included. Other
additional cost from this project were the start-up cost of materials. Revenue was generated
based on provider engagement and billing of the CPT code 99497 for Advance Care Planning.
No financial compensation to the subjects was provided for discussing ACP with their
provider. However, patients who participated in the Five Wishes seminar were given a free copy
of the AD known as Five Wishes. To purchase this AD as an individual, the patient would have
paid five dollars. The practice obtained copies of Five Wishes for $1 per copy. The cost of 120
copies of Five Wishes, along with a total 1,200 photocopies of the invitational flyer, and the cost
of the Five Wishes supplemental DVD, was close to the estimated cost of $240. Participation in
the seminar did not require completion of the Five Wishes AD but only one copy of Five Wishes
was given to each participant.
FIVE WISHES 25
Intervention
Before implementation, the three providers involved were given education on shared
decision-making skills. This education was presented at the practice meeting along with a one-
page summary on the Four Habits of Communication (Appendix D). Providers were asked if
they read the summary with all affirmative responses. At check in, every patient with an office
appointment was asked three kiosk enabled questions to determine their interest in ACP
(Appendix E) and given a paper flyer with information about the Five Wishes Seminar by the
secretary (Appendix F). The screening questions asked at each appointment were: if they have
an advance directive, if they know what an AD is and if they want to discuss an advance
directive at that visit. The responses to these questions were uploaded to the office note by the
medical assistant for the providers to see in the EHR. The process of an EHR notification acted
as a research supported reminder to providers and efficiently communicated the patient’s interest
in ACP. Even if the patient was interested in ACP, it was still up to the provider to start that
discussion. In addition, these questions served as a successful “ice breaker” to what is known to
be a difficult topic. If time constraints existed, the provider could suggest the patient return for a
separate office visit to specifically discus ACP or attend the Five Wishes Seminar. If the patient
was not interested, the provider could still decide to engage in an ACP discussion or simply
remind the patient about the Five Wishes Seminar. Providers documented an ACP discussion by
ICD-10 coding, and it was at their discretion to bill that the discussion qualified for a CPT billing
code.
The invitational flyer for the Five Wishes seminar was given to every patient (Appendix
F). The flyer provided information on location, date and time of the Five Wishes Seminar. The
flyer included a statement to encourage patients to bring a loved one to the seminar. At the
FIVE WISHES 26
seminar, consent was signed, and a pre-seminar questionnaire completed with Likert Scaled
response, before watching a short 30-minute video created by the makers of Five Wishes. After
the video, patients were encouraged to informally ask an acute care nurse practitioner questions
about end of life care or the Five Wishes AD. After the seminar was completed, the same
questionnaire was given again to the participants. This questionnaire was intended to
qualitatively assess a change in the perceived value of ACP after exposure to the educational
seminar (Appendix B). Completion of Five Wishes was not required, and this was stated at
every seminar.
Outcomes to be Measured
The outcomes measured in this project included provider engagement in ACP, percentage
of existing ADs and perceived value of the Five Wishes Seminar. The first outcome was
evaluated by the number of ACP discussion, documented by ICD-10 coding compared to the
number of ACP discussion at this same location, 12-weeks prior to project implementation. The
second outcome regarding existing ADs, was quantitatively assessed and documented by the
medical assistant in a consistent location within the EHR. This was double checked during data
retrieval and then reported as a percentage of patient encounters. Demographic information
about the patient population during the study period was also evaluated and included, age,
gender, marital status, employment status, ethnicity and race. Given the control was the same
population of patients, it was assumed to be the same cohort. A chart audit of participation in
ACP, was assessed before and after the study via ICD-10 and CPT billing claims.
The third outcome measured patients’ perceived value of the nurse practitioner led
educational session on the specific AD known as Five Wishes. This outcome was evaluated
FIVE WISHES 27
through the mean questionnaire responses pre and post Five Wishes seminar with the mean
Likert scores analyzed for statistical reliability via a paired t-test (Appendix B).
Project Timeline
The project timeline first started with an assessment of the need for this project in the
practice and the owners’ interest in supporting an ACP project. A table of the timeline is noted
in Figure 3. Once the evidence-based research had been reviewed, a project was developed, and
SWOT concerns addressed to improve participation and success. Development continued with a
review of the literature and assessment of cost versus benefit. After reviewing the evidence-
based research, a plan was developed that includes the evidence that supports successful
ACP. The SWOT concerns were addressed by engaging “buy in” from ancillary staff and the
providers. Unfortunately, many of the threats and weaknesses could not be addressed, such as
cultural perceptions about end of life care and office geography.
Next, the project was implemented using PET to guide design. The 12- week project
started on September 2
nd
and end November 22, 2019. The Five Wishes seminars started the
first Thursday after implementation. One planned seminar was cancelled due to equipment
malfunction. Evaluation began after the project had been implemented with the data evaluated
after completion and compared to the 12-weeks before implementation. Seminar attendance and
questionnaires responses were placed into an Excel spreadsheet for easier manipulation with
SPSS (Appendix G).
Resources Needed
Resources needed for this project were paper copies of the questionnaires and color
copies of the invitational flyer. The AD Five Wishes cost $1.00 per copy and a copy of the
FIVE WISHES 28
educational Five Wishes DVD was purchased for $24.95 plus tax. The practice purchased 100
copies of Five Wishes in English and 10 copies each of Five Wishes in Spanish and
Russian. The current AV equipment owned by the practice was used to view the Five Wishes
DVD. Other resources needed included the office space after hours for the educational seminars
as well as SPSS software, an EHR and electronic tablet as well as resource staff such as: medical
assistants, IT staff, providers, and the office secretary. Parking at the office is free.
Results
A total of 1037 office encounters were used to assess provider engagement in ACP
discussions. Some patients were seen multiple times during the 12-week period. Although the
repeated patients were given the same questions at each visit, their responses were not always the
same. Most patients who were seen during the study period had commercial insurance, were
employed full time, married, white and non-Hispanic. Table 3 gives more specific data
regarding the demographics of the population studied. The median age of participants was 53.
The minimum age was 18 and the oldest participant was 97. Histogram confirmed an equitable
distribution among all age groups and division between men and women was 39 % and 61%,
respectively. The percentage of Medicare patients who participated was 20%. Unfortunately,
220 office encounters were excluded from data analysis due to missing responses to the three
pre-visit questions or lack of questions being uploaded into the EHR correctly. Patients who had
at least one response to the three questions uploaded into the EHR were included in the data
analysis.
Provider engagement was evaluated by Chi Square analysis and cross tabulated to the
patient response to the “check in” question regarding interest in discussing ACP . The data
results were statistically significant with a X2=205.561 and p<0.001. Cronbach’s Alpha
FIVE WISHES 29
reliability for these questions was 0.512. A total of six patients had engaged in ACP discussions
at this office location, by these same providers in the 12-weeks before implementation. At the
end of the 12-week implementation period, a total of 90 patients participated in an ACP
discussion with their provider.
The second aim was to document patients who had an existing AD. This was assessed as
a descriptive result. Prior to this intervention, there was not a consistent process in place to
record that patients had an existing AD. This QI project allowed for a consistent opportunity to
ask patients if they had an AD and document their response. The results over 12-weeks of
patient encounters showed that of the 1037 patient encounters, 237 (22.9%) of the encounters
answered the question that they had an existing AD. This number is slightly lower than other
reported percentage that estimate approximately 33% of American adults have an AD (Yakov
et.al, 2017). Given the denominator of this data evaluation was based on the number of
encounters and not individual patients, the percentage of existing ADs may be higher than 23%.
The third aim was to create a valuable, educational seminar on a specific AD known as
Five Wishes. A total of 22 people attended the seminars during the 12-week implementation
phase. One person arrived after the video started and thus was not included in the statistical
analysis. No demographic information for the Five Wishes participants was collected other than
gender. The cohort of participants included 14 females and 7 males. On one occasions, the
seminar was cancelled due to equipment malfunction. All participants were given a pre and post
questionnaire regarding their opinion about Five Wishes and ADs, in general. The same
questionnaire was given pre and post seminar with Likert scaled responses (0-5) that numerically
correlated with positive opinions about ADs. These responses were averaged and the mean
FIVE WISHES 30
responses analyzed via a paired t-test analysis comparing pre and post questionnaire responses.
Cronbach’s Alpha for this questionnaire was 0.771.
The 21 responses analyzed showed mixed statistically significance. The response to
questions 3, 4 and 6 for the pre and post Five Wishes questionnaire did have statistically
relevance with a p<0.05 (Table 3). However, mean scores for both the pre and post
questionnaire responses were positive and averaged over 4. The first question was not analyzed
because it was a statement about an existing AD and thus post questionnaire responses were
unchanged. Question 4 stated “I think Five Wishes is an advance directive I will use” and pre
and post p value for this response was <0.05. The pre mean score for this question was 3.43 and
post mean score was 4.62 suggesting the seminar was successful in meeting the objective of
educating patients on the value of Five Wishes as an AD. The questionnaire responses, albeit
positive, lacked variability as most of the participants already had a favorable opinion of AD,
indicating a ceiling effect. In addition, the providers subjectively felt the ACP seminar was an
added value to the practice. Given most of the patients seen during implementation, work full
time, this seminar may have been more successful if held on a weekend instead of mid-week at
5pm.
In the end, there was a significant improvement in ACP discussions with the EHR
reminders of patient’s interest in ACP. In total, 116 patients answered that they wanted to
discuss ACP at that visit, yet only 51 (44%) of those who answered yes, had a provider engage in
an ACP discussions. Surprisingly, 39 (4%) patients who had answered “no” to their interest in
discussing ACP, still had a provider engaged in an ACP discussion. This suggest that patients
are 10 times more likely to have an ACP discussion if simply asked about interest in ACP. The
elicited interest and visual reminder of the responses in the EHR did motivate provider
FIVE WISHES 31
engagement. Most patient encounters (87.3%) answered that they did not want to discuss ACP
however, 56% of these patients who did not want to discuss ACP also did not know what an AD
was. This creates an opportunity for future ACP research to work on better methods to educate
the general population about ADs and normalize discussions about ACP in primary care.
The other value of this study design is the benefit of eliciting interest about the topic of
end of life care with a non-threatening process. Patients who wanted to discuss ACP had the
ability to confirm their interest by a simple intake response which gave the provider an “ice
breaker” to start the difficult conversation about dying and end of life care. It also allowed
complete inclusion of everyone in this opportunity, not just aging and medically ill. Lastly, just
by asking the questions, the topic and terminology was introduced to patients who may otherwise
never hear these terms. Primary care is the obvious place for ACP discussions to originate given
the close relationships garnered in this setting. We must continue to find creative ways to
engage patients in this important but challenging topic.
Discussion
The implications to clinical practice are to change when ACP is discussed in primary
care. This project demonstrated an easy and financially sustainable process utilizing technology
that is already in place. Making the terminology and opportunity to discuss ACP available at
every primary care encounter, changes the paradigm of who we assume needs this discussion but
most importantly, normalizes ACP. Waiting to address ACP when someone is medically ill or
faced with a terminal diagnosis is too late. This project successfully demonstrated how ACP can
easily be incorporated as a routine part of the primary care experience. End of life care will
always be a difficult topic to discuss but offering the information to everyone, can normalizes the
discussion and improve AD implementation.
FIVE WISHES 32
The healthcare policy most needed to continue to support ACP, is to continue to
incentivize provider engagement and patient participation in ACP. For example, many Medicare
recipients do not realize that they can make an appointment with their primary care provider just
to discuss ACP. Although this is already incentivized for the provider, it could also be
incentivized for the patient. Annual wellness visits include numerous questions about safety,
socioeconomic, existing AD and care needs. However, in clinical practice, the AD component
of this questionnaire gets buried by the other areas of concern, like falls and referrals to
specialist. A specific, patient incentive to see a provider just for ACP, either through a monetary
or access reward, could help perpetuate this discussion.
Implications for executive leadership are to financially support clinical processes that
facilitates this paradigm shift of asking every adult about ACP at every office location. In
addition, with better documentation of existing AD, a process to communicate this existing
document with specialist and hospitals needs to be implemented. Knowing patients have an AD
is only the first step in using ADs. Because research also supports the value of a team-based
approaches to ACP, leadership could facilitate ACP through advertising that patients can make
appointments just to discuss ACP and continue free ACP seminars facilitated by other specialist
such as spiritual leaders, social workers, attorneys, etc. The normalization of ACP is supported
by making ACP a separate “product line” advertised and supported with a variety of resources.
Implications for quality and safety are in utilizing healthcare resources responsibly and
improve our ability to meet the standards of care. This primary care practice is part of an
Accountable Care Organization where the quality of care impacts reimbursement and ACP is a
quality measure that impacts outcomes. ACP address quality in an ACO through reduction in
FIVE WISHES 33
unnecessary healthcare spending without impacting care quality. The healthcare community has
a responsibility to demonstrate quality while being good stewards of healthcare resources.
Sustainability and Future Scholarship
There was strong, financial sustainability demonstrated by this project. Approximately
$4000 in revenue was generated by this process. The process of utilizing the current electronic
health resources created a seamless process to continue to normalize the terminology of ACP and
engage more patients in an ACP discussion. Medicare reimbursement as well as some
commercial insurance reimbursement of ACP engagement allows this project to continue to be
sustainable. Future scholarship should focus on creative ways to educate and engage more
patients in understanding the value of AD and ACP. This project demonstrated that most people
did not want to discuss ACP, but normalization of these discussion, could change this pervasive
opinion. Normalization can only be achieved by continuing research that address ACP in
primary care.
Conclusion
In summary, an ACP process is a valuable addition to any primary care practice and
especially for a primary care practice that values comprehensive care. This project added a
missing aspect to the goal of holistic care. Evidence-based research on ACP was translated into
a successful clinical process that has benefits beyond cost and most importantly, advances the
conversation about end of life care. Ultimately, a successful ACP process can normalize how
we discuss death with patients and open opportunities to better understand the value of an AD,
especially the unique AD known as, Five Wishes.
FIVE WISHES 34
Figure 1 Revised Johns Hopkins Model (Revised Johns Hopkins Model, n.d)
FIVE WISHES 35
Figure 2 Methodology Map

FIVE WISHES 36
Figure 3 Project Timeline
Nov/Dec 2018:
Owner
interest/Needs
Assessment
March-June
2019 SWAT
Analysis/EBR
assessed
June-August
2019: Staff "buy
in", Process
created, resources
obtained
September 2019-
December 2019:
Implementation of
project
January-May
2020: data
analysis and
evaluatation of
implementation
process for
practice wide use

FIVE WISHES 37
References:
Advance Directives. (n.d.). Retrieved from
http://www.marylandattorneygeneral.gov/Pages/HealthPolicy/AdvanceDirectives.aspx
Aging with Dignity. (2012, July 12). Retrieved February 16, 2019, from
https://www.rwjf.org/en/library/research/1997/01/aging-with-dignity.html.
Baik, D., Cho, H., & Creber, R. M. (2018). Examining Interventions Designed to Support Shared
Decision Making and Subsequent Patient Outcomes in Palliative Care: A Systematic
Review of the Literature. American Journal of Hospice and Palliative
Medicine®,36(1), 76-88. doi:10.1177/1049909118783688
Bond, W. F., Kim, M., Franciskovich, C. M., Weinberg, J. E., Svendsen, J. D., Fehr, L. S., . . .
Asche, C. V. (2018). Advance Care Planning in an Accountable Care Organization Is
Associated with Increased Advanced Directive Documentation and
Decreased Costs. Journal of Palliative Medicine,21(4), 489-502.
doi:10.1089/jpm.2017.0566
Dearholt, S. & Dang, D (2018). Johns Hopkins Nursing Evidence-Based Practice Model and
Guidelines. Indianapolis, IN: Sigma Theta Tau International.
Douglas, R., & Brown, H. N. (2002). Patients Attitudes Toward Advance Directives. Journal
of Nursing Scholarship,34(1), 61-65. doi:10.1111/j.1547-5069.2002.00061.x
E-Clinical Works (ECW) [Program documentation]. (n.d.). Retrieved April 1, 2019.
Forcino, R., Paul, B. J., James, O., Roger, A., & Molly, C. (2018). Using CollaboRATE, a brief
patient-reported measure of shared decision making: Results from the three clinical

FIVE WISHES 38
settings in the United States. Health Expectations,21, 82-89.
doi:10.1111/hex.12588
Hayek, S., Nieva, R., Corrigan, F., Zhou, A., Mudaliar, U., Mays, D., . . . Ilksoy, N. (2014). End-
of-Life Care Planning: Improving Documentation of Advance Directives in the
Outpatient Clinic Using Electronic Medical Records. Journal of Palliative Medicine,
17(12), 1348-1352. doi:10.1089/jpm.2013.0684
Hilgeman, M. M., Uphold, C. R., Collins, A. N., Davis, L. L., Olsen, D. P., Burgio, K. L., . . .
Allen, R. S. (2018). Enabling Advance Directive Completion: Feasibility of a New
Nurse-Supported Advance Care Planning Intervention. Journal of Gerontological
Nursing, 44(7), 31-42. doi:10.3928/00989134-20180614-06
Hinderer, K. A., & Lee, M. C. (2014). Assessing a Nurse-Led Advance Directive and Advance
Care Planning Seminar. Applied Nursing Research,27(1), 84-86.
doi:10.1016/j.apnr.2013.10.004
Jensen, B. F., Gulbrandsen, P., Dahl, F. A., Krupat, E., Frankel, R. M., & Finset, A. (2011).
Effectiveness of a short course in clinical communication skills for hospital doctors:
Results of a crossover randomized controlled trial (ISRCTN22153332). Patient
Education and Counseling, 84(2), 163-169. doi:10.1016/j.pec.2010.08.028
Life in USA. Death in USA. (n.d.). Retrieved from http://www.lifeintheusa.com/death/
Maryland Attorney General. (n.d.). Retrieved from
http://www.marylandattorneygeneral.gov/Pages/HealthPolicy/AdvanceDirectives.aspx
FIVE WISHES 39
Pelland, K., Morphis, B., Harris, D., & Gardner, R. (2019). Assessment of First-Year Use of
Medicare’s Advance Care Planning Billing Codes. JAMA Internal Medicine.
doi:10.1001/jamainternmed.2018.8107
Raghavan, D. (2014, July 03). Most Educated Places in America. Retrieved April 13, 2019, from
https://www.nerdwallet.com/blog/mortgages/home-search/educated-places-
america/?trk_location=ssrp&trk_query=most educated city in
US&trk_page=1&trk_position=1
Rao, J. K., Anderson, L., Lin, F. C., & Laux, J. (2014). Information for CME Credit —
Completion of Advance Directives Among U.S. Consumers. American Journal of
Preventive Medicine, 46(1). doi:10.1016/s0749-3797(13)00608-9.
Reinhardt, J. P., Chichin, E., Posner, L., & Kassabian, S. (2014). Vital Conversations with
Family in the Nursing Home: Preparation for End-Stage Dementia Care. Journal of
Social Work in End-Of-Life & Palliative Care, 10(2), 112-126.
doi:10.1080/15524256.2014.906371
Revised Johns Hopkins Model [Digital image]. (n.d.). Retrieved from
https://www.hopkinsmedicine.org/evidence-based-practice/ijhn_2017_ebp.html
Ruparel, M., Quaife, S. L., Ghimire, B., Dickson, J. L., Bhowmik, A., Navani, N., . . . Janes, S.
M. (2019). Impact of a Lung Cancer Screening Information Film on Informed Decision-
making: A Randomized Trial. Annals of the American Thoracic Society, 16(6), 744-751.
doi:10.1513/annalsats.201811-841oc
FIVE WISHES 40
Splendore, E., & Grant, C. (2017). A nurse practitioner–led community workshop. Journal of the
American Association of Nurse Practitioners, 29(9), 535-542. doi:10.1002/2327
-6924.12467
Tripken, J. L., Elrod, C., & Bills, S. (2016). Factors Influencing Advance Care Planning Among
Older Adults in Two Socioeconomically Diverse Living Communities. American
Journal of Hospice and Palliative Medicine®,35(1), 69-74.
doi:10.1177/1049909116679140
U.S. Department of Health and Human Services. (n.d.) Retrieved from
https://health.gov/communication/literacy/issuebrief/
Van Wert (2018, August 19). Four key components of a successful advance care planning
program. Retrieved April 27, 2019 from https://vyncahealth.com/four-keu-components
-successful-advance-care-planning-program/
Verhovshek, J. (2016). The Medicare Advance Care Planning Benefit. Retrieved from
https://www.aapc.com/blog/34941-the-medicare-advance-care-planning-benefit/
Whelan, D. (2013, June 19). ObamaCare Dives Into End-Of-Life Debate. Retrieved April 11,
2019, from https://www.forbes.com/2009/07/24/obamacare-medicare-death-business-
healthcare-obamacare.html#15bc567d4ef6
FIVE WISHES 41
Appendices
Appendix A Evidence Table
Article Author Evidence Sample Findings Observable Limitations Evidence
Level/Quality
Arti
cle
Author
Evidence
Type
Sample,
Sample
Size,
Setting
Findings that
help answer
the EBP
Question
Observable
Measures
Limitations
Evide
nce
Level
&
Qualit
y
Arti
cle
#1
Hayek,
et. al.
(2013)
Prospecti
ve QI
study
588 patient
charts were
screened
with 157
meeting
criteria for
AD
documenta
tion
The study
implemented
an EHR based
reminder for
patients with
eligible
chronic
medical
conditions. An
EHR based
reminder does
improve
providers
documentation
of AD and
ACP. The
study used the
EHR to
implement a
reminder
process and
likely, a
similar
reminder will
be needed for
my project.
An EHR based
reminder for
providers to
address
ACP/ADs did
improve
documentation
of ADs.
However, more
than one
reminder
correlates with
better
implementation.
The authors
also suggest
that a dedicated
location to
documente AD
improved
documentation.
These are all
factors that will
need to be part
of my project to
address
provider
engagement in
ACP. Provider
engagement is
one of my
SWOT
concerns.
Primary care
providers were
given
reminders to
address
AD/ACP for
only patients
who met
criteria for
chronic
medical
problems
however, all
patients were
encouraged to
complete an
ACP. People
with end of life
and serious
medical
problems may
be more likely
to complete
ADs and thus
may explain
the significant
participation.
The sample
size was small.
Interestingly,
the ACP
conversations
were via
medicine
IIA
FIVE WISHES 42
residents in
training rather
than by
primary care
providers with
long standing
relationships.
This may be a
function of
excellent
patient
centered
communication
. Regardless,
there is clear
support to
having
electronic
reminders for
my AD/ACP
project.
Arti
cle #
2
Hinder
er, K.,
et, al.
(2014)
Quasi-
Experim
ental
86
voluntary
participant
s from the
community
age 20-89
Community
participants
were offered
free,
informational
sessions about
Five
Wishes. This
study mirrors
my project by
evaluating a
nurse lead
informational
session on
Five Wishes
AD
planning. Find
ings did not
correlate with
a change in
ADAS scores
(patients’
attitude) about
ACP post
educational
seminar. How
ever, most
found the
seminar useful.
Advance
Directive
Attitude Survey
(ADAS) score
ranged from 16-
54 with a higher
score
correlating with
more favorable
attitudes
towards
ACP. The
study found no
change in
ADAS scores
pre, post and 1
month after
educational
session.
However, after
the session,
97.7% reported
they were likely
to complete an
AD. The lack
of change in
ADAS score
may be related
to 40.7% had
ADAS scores
were measured
prior,
immediately
post and 1
month after
educational
intervention.
No data on
implementatio
n of AD one
month after the
session was
measured. Bec
ause this took
place in a
community
setting rather
than in
conjunction
with a primary
care practice,
patients who
already
understood and
valued ACP,
may have
disproportionat
ely represented
IIB
FIVE WISHES 43
This supports
my plan to
incorporate
AD (Five
Wishes)
informational
sessions after
office hours
and open to
patients and
loved ones to
attend as an
intervention to
improve
understanding
and give more
opportunities
to answer
questions
about ACP.
been a surrogate
decision makers
and already had
a positive
attitude, 30%
already had an
AD and nearly
69% had
already
discussed ACP
with a
provider. Despi
te this,
participant post
intervention
survey found
the majority
82.6% did find
the seminar
useful. This
supports the
need for
informational
sessions in my
project but in
conjunction
with SDM and
provider
support. The
study also
included a
demographic
instrument
created
specifically for
the study and
likely will also
be needed in
my project.
Because the
ADAS tool is
valid and
reliable, it will
be used to
measure
attitudes about
ACP in my own
5 Wishes
informational
session.
the sample of
participants.
Assessing a
larger cohort of
primary care
patients’
understanding
of ACP before
and after could
be valuable to
see if this type
of
informational
session
improves
primary care
patients’
attitudes, and
knowledge of
ACP and AD
implementatio
n.
FIVE WISHES 44
Arti
cle
#3
Tripke
n, J.L,
et. al.
(2018).
Qualitati
ve Cross-
sectional
survey
77 adults
55 years
and older
were
surveyed
from two
different
socioecono
mic living
communiti
es
Adults living
in High
Income
Eligible (HIE)
were more
likely to
engage in ACP
compared to
people in an
Affordable
Housing
Communities
(AHC)
Because ACP is
such a complex
process, this
article
highlights that
socioeconomic
status does
impact
ACP. This
encourages the
need for my
project to target
at risk groups
who may be
less informed
about ACP.
Given we know
ACP
substantially
impacts end of
life care, this
socioeconomic
group needs
additional
focused
outreach to
reinforce the
value of ACP.
Education
levels differed
significantly
among the two
groups and
correlated with
socioeconomic
status. I
suspect
exposure to
information
about ACP is
more likely to
have occurred
with people in
a higher
socioeconomic
and
educational
level. For
example, many
people fill out
an advance
directive when
they write their
living will.
Less educated
people may be
less likely to
have a living
will and miss
the opportunity
to learn about
AD. Interestin
gly, the study
evaluated self-
reported health
status of each
group. The
group least
likely to
complete an
ACP were also
the group that
reported the
poorest health
status. This
highlights that
ACP may be a
function of
repeated
IIIA
FIVE WISHES 45
exposure to the
information
and providers
may be
unintentionally
avoiding ACP
to this subset
population. If
you have
poorer health,
you
theoretically
would have
more contact
with a provider
and thus more
opportunities
to discuss
ACP.
Therefore, I
am opening my
project to
everyone.
With repeated
exposure to the
information
comes equal
opportunity for
everyone to
create an AD.
Lastly, despite
these
differences in
ACP
knowledge,
both groups
had similar
attitudes and
desires
regarding
death and
dying.
Arti
cle #
4
Splend
ore, E.
et. al,
(2016)
Quasi-
experime
ntal
Convivenc
e sample of
40 (23
from the 1
st
workshop
and 17
from the
second)
Study
concluded that
a Five Wishes
educational
workshops in a
community
setting
increased
Pre-workshop
questionnaires
with 19 self-
reported and
open-ended
questions on
understanding,
perception of
There was not
a standardized
questionnaire
nor was the
completion of
AD
verified. Verif
ication of an
IIB
FIVE WISHES 46
participant
s over the
age of 18
from a
rural town
in
Pennsylvan
ia attended
an ACP
workshop
held
twice. No
statistical
difference
in the two
groups that
attended
the
workshops.
understanding,
completion
and discussion
of ACP/AD
among
participants
and their
family
members. This
AD workshop
on discussing
Five Wishes is
part of my
DNP project
and thus the
implementatio
n method of
this study is
valuable.
importance and
dissemination
of ACP status
was measured
via Likert type-
1
questions. Post
workshop
evaluations
were also self-
reported
questionnaires
and then a 1
month follow
up phone call
questionnaire
with 8 self-
reported
answers
regarding the
ACP process,
implementation
and perception
of importance
was
completed.
AD for my
project is
important as
many studies
show patients
agree with the
value of ACP,
but fewer make
the step to
complete an
AD and thus
AD
documented
completion
will be a
measured
value for my
project. Prima
ry care
providers were
not part of this
ACP process in
this study as it
was a
community
project. In
addition, the
study was
supported by
Aging with
Dignity who
developed the
Five Wishes
tool creating
some potential
bias.
Arti
cle #
5
Forcin
o, R.
et. al.
(2017)
Quasi-
experime
ntal
Survey
3 separate
primary
care
practice
sites in the
US asked
patients
over 18,
post visit,
the
CollaboRA
TE patient
survey tool
to measure
The study was
intended to
evaluate
CollaboRATE
scores for 3
outpatient
primary care
practice in 3
different
geographical
locations to
assess in real
time, a
patient’s
Results
conclude that
CollabRATE
can be used in a
diversity of
primary care
settings and the
short
measurements
tools reduce
some of the
administrative
burden of
collecting
Validity and
reliability of
the
CollaboRATE
tool is noted in
a “simulation
sample”. This
study has value
in its ability to
assess shared
decision
making
immediately
after a patient
IIA
FIVE WISHES 47
perceived
Shared
Decision
Making
(SDM).
experience of
SDM at their
primary care
provider’s
office.
data. This
could be a
valuable tool to
assessing
patient’s
perception of
SDM for my
project. A
strong sense of
SDM is needed
for AD
planning
success. Using
this tool could
evaluate if the
providers in my
practice are
perceived as
participating in
SDM. .
encounter to
give faster
feedback to
providers. This
tool might be
more
beneficial if
administered
via an
electronic
platform to
give immediate
feedback and
to have
provider adjust
their approach
to ACP. SDM
is essential for
primary care to
effectively
create AD.
Arti
cle #
6
Jensen,
B. F.
et. al
(2011)
RCT,
cross
over
72
hospital-
based
doctors in
various
specialties
were
randomize
d to IG vs
CG for a
20-hour
Four
Habits
Communic
ation
training vs.
no training
Statistically
significant
improvement
in 4HCS score
among IG and
the duration of
patient
encounter did
not change
significantly.
Patient
satisfaction
surprisingly,
did not
change.
4HCS is
reliable and
valid tool that
uses a 23-item
scale to assess
effectiveness in
communication.
This study
validates the
benefit of the
Four Habits
Model in
improving
provider
communication.
Although an
older article,
this was
included
because it is a
true RCT that
evaluated 4
Habits among
many
physician
specialties and
not just in
mental health.
The
participants
received a Four
Habits
reminder to
carry with
them which I
may also add
to my
project. It was
surprising that
the IG did not
have
significantly
longer patient
encounters
IB
FIVE WISHES 48
compared to
CG as many
providers feel
patient
centered
communication
is more time
consuming.
This alone
supports the
value of
improving
provider
communication
and will be
used to
encourage
providers in
my project to
use the 4H
skills. Howeve
r, the authors
do
acknowledge
that the shared
decision-
making aspect
of the process
is the most
time
consuming. I
was surprised
that patient
satisfaction did
not change in
this study’s
analysis. This
could be
related to the
environment as
the providers
were hospital
based and not
in a primary
care practice
where patients
have a greater
expectation of
relationship
with their
FIVE WISHES 49
providers.
Arti
cle #
7
Baik,
D. et.
al.
(2019)
Qualitati
ve study-
literature
review
Systemat
ic
Review
12 Studies
were
reviewed
for
interventio
ns that
support
Shared
Decision
Making
(SDM) and
subsequent
patient
outcomes
in
palliative
care
Although the
authors
conclude
inconsistent
findings
regarding
SDM
interventions
and
patient/caregiv
er outcomes,
this article is
valuable to
my project
because it lists
the common
SDM
interventions
used in other
research.
MMAT tool
was used to
assess the
quality of
studies and
validate rigor.
SDM was
categorized into
4 main areas:
technology
enabled
delivery modes,
print material,
palliative care
consultation
and structured
meetings. Tech
nology enabled
SDM tools were
more frequently
used. The
author suggests
the biggest
weakness is
lack of
individualized
SDM tools and
thus a factor to
consider in
establishing
SDM for my
project.
The review
highlights a
need for
validated and
reliable
instruments to
assess SDM
interventions.
Thus, I will
seek what
SDM tool is
most validated
in preparation
for my project.
VB
Arti
cle
#8
Bond,
W. et.
al.
(2018)
Quasi-
experime
ntal Case
Control
Matched
Study
Retrospecti
ve
evaluation
of 325
Medicare
cases with
documente
d AD and
had died
were
matched to
similar 325
Medicare
control
Cases with AD
had fewer
inpatient
admissions,
and inpatient
days but
slightly more
CHF and
COPD. Even
after
accounting for
the cost of
implementing
an ACP
Unpaired t test
and Chi
Squared test
used to evaluate
the two
groups. A
multiple
imputation
method was
used to fill out
outcomes
variables in
patients who
died before the
The Health
Catalyst
database,
IDEA, is
HIPPA
protected, but
not used
routinely in all
ACO
practices. The
addition of this
database may
be useful for
my DNP
IIA
FIVE WISHES 50
cases
without an
AD in an
ACO in
Illinois.
program, the
net savings
over 12
months to
Medicare
expenditure
was
$1,572,330
(104% Return
on
Investment).
12 months. The
project used
ACO data, an
ACP facilitator
called IDEA
(database to
track ACP) and
EHR to analyze
the data. Cost
savings was
statistically
significant in
the ACP group.
Given my
organization
participate with
an ACO, the
cost savings
aspect of
creating an
effective ACP
program is
strongly
supported.
project but will
require partner
“buy in” to
purchase this
software that is
external to the
EHR. This
does validate
the importance
of having AD
documents
easily
accessible in a
secure location
will be an
important
teaching aspect
in
implementing
my project.
The American
Bar
Association
also offers a
free website to
upload ACP
and will be
discussed at
the informatio
nal sessions.
The authors do
acknowledge
that cost
savings is not
the goal of an
ACP program
and many other
aspects to this
retrospective
study, like
family support,
could not be
measured.
Arti
cle
#9
Reinha
rdt, et.
al.
(2014)
RCT
110 family
Surrogates
from
nursing
home with
a family
member
PCT face to
face IG patient
surrogates
were
significantly
more satisfied
with their
McNemar’s test
was used to test
the hypothesis
that the IG had
more advance
directives in
place over time.
Limitations of
this study were
minimal. It
was a strong
design but
given the
patient
IA
FIVE WISHES 51
with
dementia
were
randomly
assigned to
interventio
n (n-58)
(face-to-
face
meeting
and follow
up calls
from PCT)
vs
compariso
n group
(n=52)(rou
tine
nursing
home
care).
loved ones’
care and had
more advance
directive
planning
documented
compared to
control. The
IG was more
likely to have
a MOLST on
record and
have a DNR,
DNI or DNH
order
included.
Surrogate
satisfaction was
measured at
baseline, 1, 3
and 6
months. This
highlights the
benefits of
including loved
ones in ACP as
well as the
benefit of face
to face
conversations
about ACP.
Therefore, my
project will
need more than
simple
education. Prov
iders will need
to “buy in” to
the importance
of ongoing
communication
and face to face
discussions.
population, it
could not
directly
assess how the
PCT impacted
the patient. It
does highlight
the benefit of a
team approach
to advance care
planning is
needed.
Arti
cle
#10
Hilgem
an, et.
al.
(2018)
RCT
50 VA
patients
randomize
d to a
NSACP vs
usual care
(referred to
a social
worker)
A formal,
nurse led
program that
taught patients
the risk,
benefits and
alternatives of
life sustaining
procedures
(RBA). The
results show
the IG were
more likely to
decline life
sustaining
treatment, had
more patient
satisfaction,
participant
retention and
treatment
fidelity
Demographic
data, past
experiences
with ACP and
desire for help
completing an
AD as well as
information
about RBA was
collected via a
questionnaire.
Only 4
participants had
prior
discussions
about ACP. The
majority wanted
more
information
about RBA than
just ACP. The
IG intervention
was 46 minutes
The RBA
information
was provided
by a RN via a
slide show and
with printed
handouts. Giv
en the CG
usually does
AD planning
with a social
worker, it
validates the
need for the
ACP to be
done by a
medical
provider who
can answer
question about
RBA. Thus,
the providers
in my project,
IB
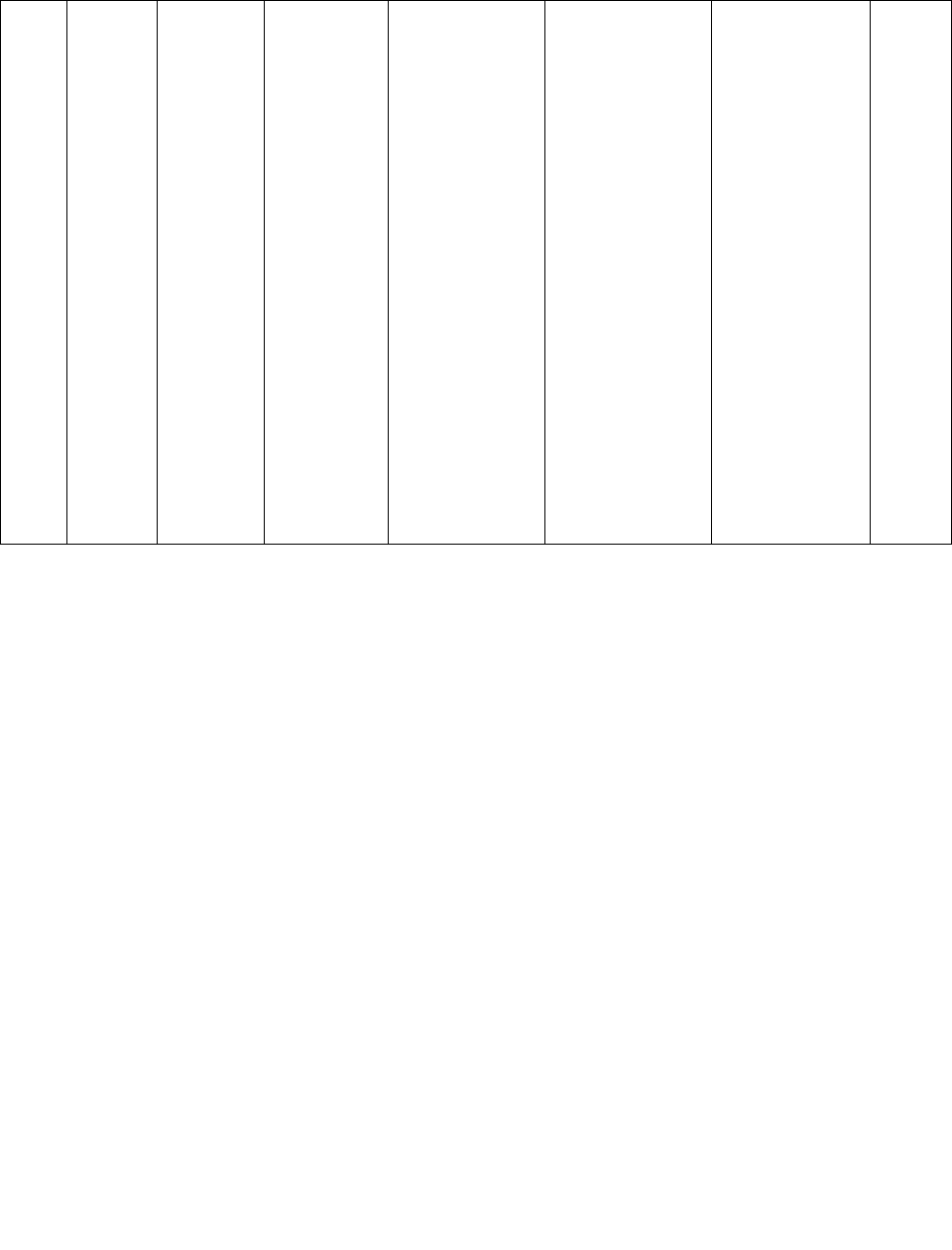
FIVE WISHES 52
compared to 29
in the CG. This
is valuable to
my project, as
the biggest
limitation to
providers
discussing ACP
at every
appointment, is
time. Thus,
patients in my
project will be
offered an
appointment to
just discuss
ACP as well as
the weekly,
free,
informational
session.
will be
reminded to be
prepared to
discuss RBA
when engaging
in ACP.
Appendix B FIVE WISHES SEMINAR QUESTIONAIRE
Please answer the following questions as:
5=Strongly Agree, 4= Agree, 3= Neutral, 2= Disagree 1= Strongly Disagree 0= NA
___________1. I have previously completed an advance directive
___________2. I believe an advance directive is very important
___________3. I feel an advance directive will help guide my family
___________4. I think Five Wishes is an advance directive I will use.
___________5. I plan to discuss my advance care planning desires with my family and loved
ones.
___________6. I plan to discuss my end of life desires with my provider.
FIVE WISHES 53
Appendix C Consent to participate
Five Wishes Educational Seminar Comprehensive Primary Care
5413 West Cedar Lane, Suite 203c, Bethesda MD 20814
1. PURPOSE AND BACKGROUND
Amanda Bridges, CRNP and The George Washington University are conducting research on
advance directives. The purpose of your participation in this research is to help the researcher
improve education about the advance directive, Five Wishes.
B. PROCEDURES If you agree to participate in this research study, the following will
occur: You will be asked to answer a pre and post questionnaire. You will watch a short 30-
minute video on the advance directive known as Five Wishes. Total time commitment is
estimated to be 1 hour and 30 minutes.
C. RISKS There are minimal risk to participating in this study. Some patients may be
emotionally upset about a discussion about end of life care and death.
D. CONFIDENTIALITY The records from this study will be kept as confidential as
possible. No individual identities will be used in any reports or publications resulting from the
study. All questionnaires will be destroyed after analyzed. Research information will be kept in
a locked cabinet. Only research personnel will have access to the questionnaires.
E. BENEFITS OF PARTICIPATION The anticipated benefit of your participation in this
study is a free, copy of Five Wishes and increased understanding of this advance directive
F. VOLUNTARY PARTICIPATION Your decision whether to participate in this study is
voluntary and will not affect your relationship with Comprehensive Primary Care. If you choose
to participate in this study, you can withdraw your consent and discontinue participation at any
time without prejudice.
G. QUESTIONS If you have any questions about the study, please contact Amanda Bridges
by calling 301-869-9776.
Signature ________________________________ Date_______________________
Research Participant
_________________________________________ Date: _______________________
Amanda Bridges, MSN, ACNP-BC
School of Nursing THE GEORGE WASHINGTON UNIVERSITY [email protected] 202-994-7901
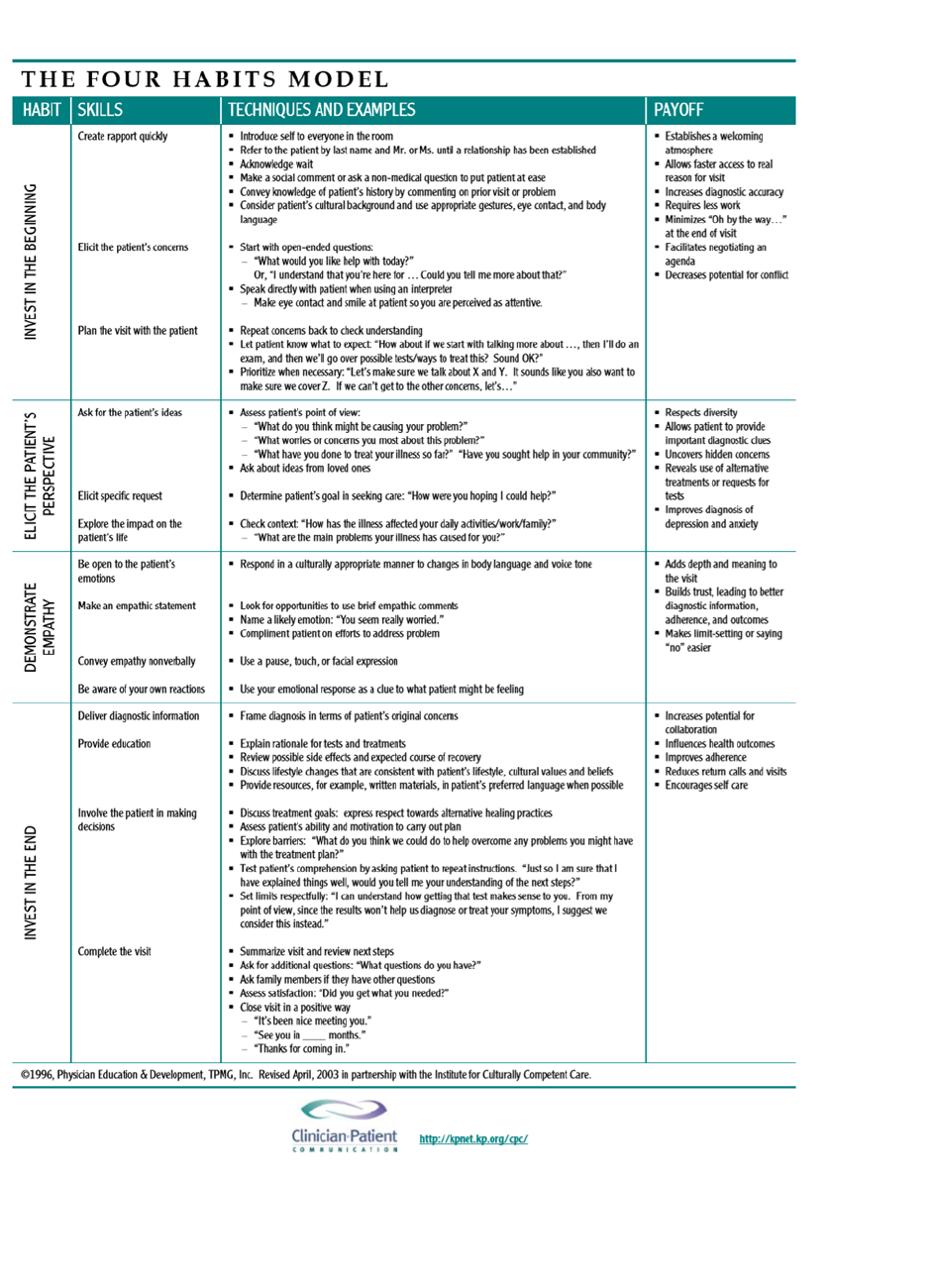
FIVE WISHES 54
Appendix D Shared Decision Making Tool

FIVE WISHES 55
Appendix E Kiosk Intake Questions
1. Do you have an Advance Directive?
2. Do you know what an Advance Directive is?
3. Do you want to discuss Advance Care Planning today?
FIVE WISHES 56
Have you designated a person to make
medical decisions for you in the event you
are unable?
Do you know what an advanced directive is?
Do you want unnecessary medical
procedures done to you in the event you
have no hope of survival?
Appendix F: Five Wishes Seminar Invitation
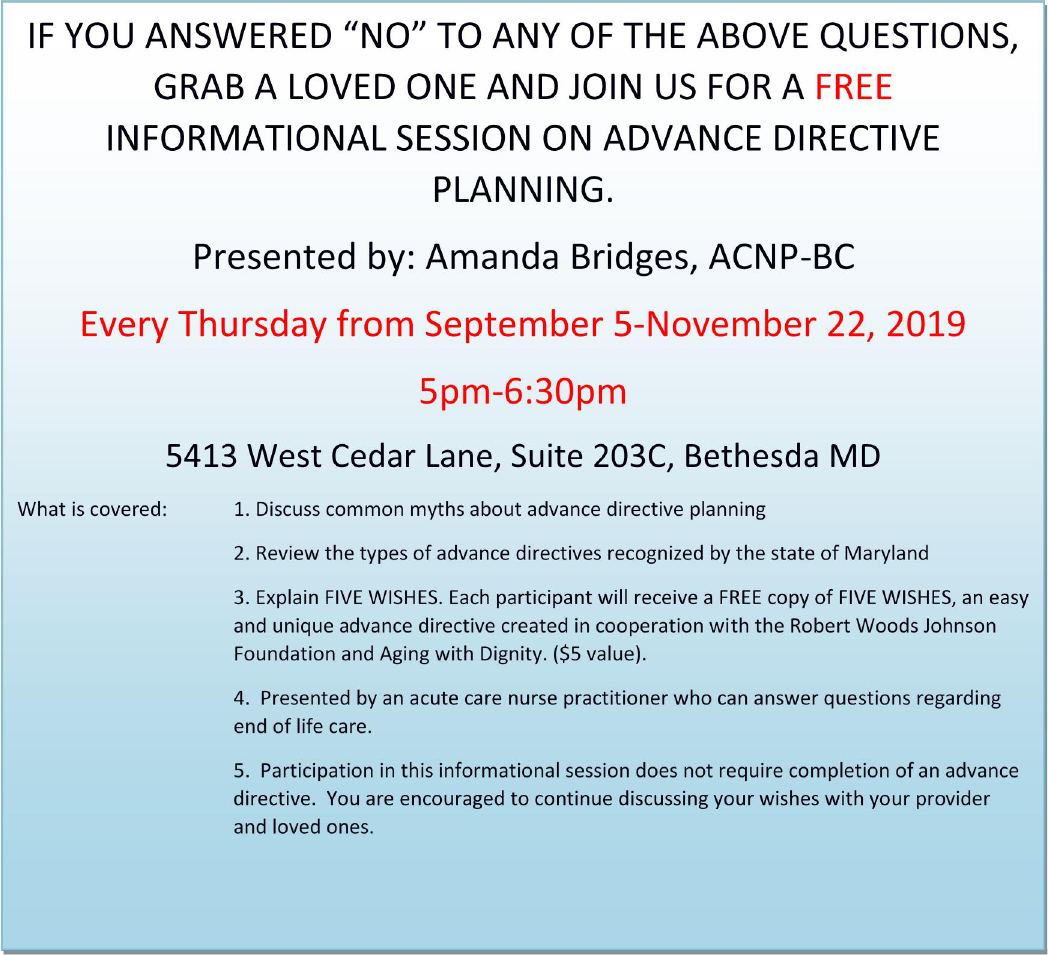
FIVE WISHES 57
FIVE WISHES 58
Appendix G: Provider Engagement in ACP Data Collection Worksheet
Patient
Initials/last
2
MR#
Q1 (1=yes, 2=no)
Q2
Q3
Age
Gender
Employee status
Marital Status
Ethnicity
Race
Insurance
Discussion took
place
?
AB3455
1
1
1
51
F
Full Time
Married
White
Non-
Hisp
anic
Comm
ercial
Yes
Data Collection Worksheet for Five Wishes Seminar (Pre/Post)
Initial
Date
Gender
(M/F)
PreQ1
PreQ2
PreQ3
PreQ4
PreQ5
PreQ 6
PostQ1
Post Q2
Post Q3
Post Q4
Post Q5
Post Q 6
EX:
AB
11/09
F
1
3
3
4
3
5
4
4
5
5
5
5
1=Strongly Disagree, 2= Disagree, 3= Neutral, 4= Agree, 5= Strongly Disagree
FIVE WISHES 59
Table 1 Cost Benefit Analysis
COST/BENEFIT ANALYSIS
ESTIMATED
COST
ACTUAL
COST
Start Up Materials
$240
$239.97
Estimated Additional Salaries
$2,100
$0
Additional Operational Cost (EHR,
utilities, Rent, etc)
Negligible
Negligible
Revenue (CPT Billing)
$6750
$4,127.27
Total
($4,410)
($3,887.30)
Table 2: Evaluation
Objectives
Evaluation
Questions
Benchmarks
Methods
Overall Program
Improve
provider
participation
in ACP
discussions
Improve
provider
discussions
about ACP
Does a solicited
opportunity for
the patient to
discuss ACP and
an EHR reminder
improve ACP
discussions?
Providers will
improve ACP
discussions by
documentation of
ICD 10 code in
the EHR
compared to prior
3 months.
Analysis of ICD
10 ACP
documentation in
the chart over 3
months
compared to
prior 3-month
control via chi-
square analysis.
Increase
patient
education
about the AD
known as
Five Wishes
Patients will
have a better
understanding of
the AD known as
Five Wishes.
Do patients
demonstrate a
change in opinion
about the value of
an AD by
attending a Five
Wishes
educational
seminar?
Five Wishes
attendance and
mean Likert
Scaled responses
to questionnaire
Likert scaled
responses
averaged pre and
post seminar
questionnaire.
Total number of
patient
participants
Process
Successfully
involved
owners of the
practice
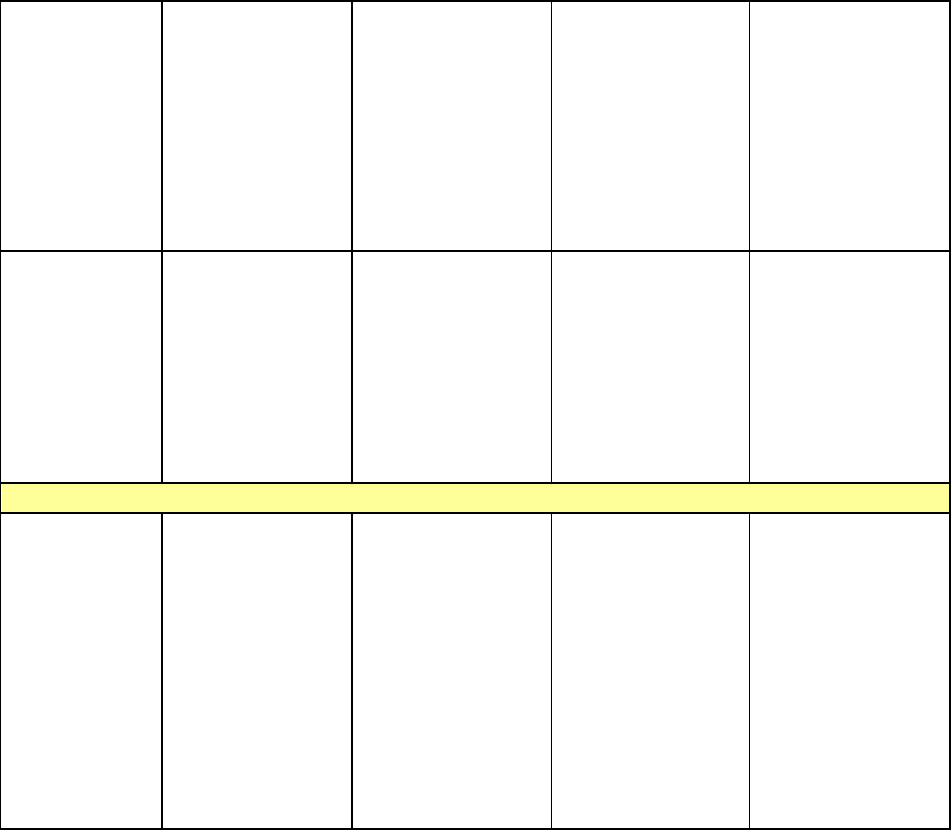
FIVE WISHES 60
Improve
provider
knowledge of
shared
decision
making
Increase provider
understanding of
basic
communication
skills to improve
shared decision
making.
Will a brief
article on the
Four Habits of
Communication
improve
providers’ ability
to engaged in
shared decision
making?
Post
implementation
analysis of
provider use of
these Four Habits
of
Communication
Providers will be
asked after the
study if they used
the Four Habits of
Communication
during this study
period.
Ancillary
staff
cooperation
Engage ancillary
staff to
implement the
new process of
asking about
ACP and
entering template
into EHR
Does a preset
template improve
medical assistant
cooperation with
entering
questionnaire
data?
Number of
patients lost
Create EHR
template and
simplify work
flow to ensure
process is easy
and seamless for
the ancillary staff
Structure
Pre-created
template for
EHR to enter
answers to
question and
engage
providers to
discuss ACP
Every patient
response to the
questionnaire
will be entered in
the EHR.
Will the
screening
questionnaire that
collects patient
response
be completed by
all the patients?
Attrition rates
Assess number of
patients seen
during the 3
months process
compared to
number of
questionnaires
completed.
FIVE WISHES 61
Table 3 Data Analysis
Demographic Characteristics and Statistics of the Sample For Provider Engagement in ACP
Discussion
Total
Sample
(N)
Frequency
(%)
Before
Intervention
Frequency
(%)
After
Intervention
Statistics
Gender
1037
Male
404
39.0%
Female
633
61.0%
Age(years)
18-40
284
27.4%
41-64
497
47.9%
65-79
217
20.9%
80-100
39
3.8%
Marital Status
Married
598
57.7%
Single
285
27.5%
Divorce
76
7.3%
Missing
42
4.1%
Widow
36
3.5%
Employment
Full Time
616
59.4%
Student
32
3.1%
Retired
51
4.9%
Self-
Employed
47
4.5%
Missing Data
265
25.6%
Not employed
26
2.5%
Race
White
723
69.7%
Black/AA
66
6.4%
Asian
66
6.4%
Other
22
2.1%
Declined
160
15.4%
Ethnicity
Non-Hispanic
743
71.6%
Hispanic
55
5.3%
Missing/Refuse
231
22.3%
FIVE WISHES 62
d
Other
8
0.8%
Insurance
Commercial
747
72.0%
Medicare
207
20.0%
Medicaid
76
7.3%
Self-
Pay/Uninsured
5
0.5%
Tricare
2
0.2%
Patient response
to at least one
question
required for
statistical
evaluation
Q1= People
who already
have an
AD/ACP
237
22.9%
Q1=People who
do not have an
AD
788
76.0%
Q1=Missing
response
12
1.2%
Q2=People who
know what an
advance
directive is
416
40.1%
Q2=People who
do not know
what an advance
directive is
586
56.5%
Q2= Missing
data
35
3.4%
Q3=Patients that
did want to
discuss ACP
116
11.2%
Q3=Patients that
did not want to
discuss ACP
905
87.3%
Q3=Missing
data
16
1.5%
Cronbach’s
Alpha for intake
0.512
FIVE WISHES 63
questions
Total ACP
discussions (all
insurances) by
ICD 10 EHR
Documentation
6 (0.005%)
90 (8.7%)
Provider
Engagement:
Discussion(see
above for
definition)
X2=205.5
61
P<0.001
Phi=0.445
Yes and Yes
51
Yes and No
65
Missing/No
and Yes
Discussed
39
No/Missing and
No Discussion
866
CPT Revenue
Anticipated if
all claims
reimburse $75
$6750.00
Actual CPT
Revenue
$4127.27
Descriptive Characteristics and Statistics of the Sample for Five Wishes Seminar
FIVE
WISHES*
Total (N)
Frequenc
y %
Mea
n
respo
nse
on
scale
(0-5)
Median
Variance
Statistics
Sig of
Paired t test
(95%
Confi)
Pre/Post
T
Sig of
sample
correlation
(pre/post)
Male
7
(33.3%)
Female
14
(66.7%)
Pre Question
1
2.76
3.00
4.290
NA
NA
NA
Post
Question 1
2.76
3.00
4.290
NA
NA
NA
Pre Question
2
4.62
5.00
0.328
0.083
-1.826
0.000
PostQ2
4.76
5.00
0.290
0.083
-1.826
0.000
Pre Question
3
4.48
5.00
0.862
0.030
-2.335
0.146
Post Q3
4.76
5.00
0.290
0.030
-2.335
0.146
Pre Question
3.43
4.00
2.857
0.003
-3.408
0.00
FIVE WISHES 64
4
PostQ4
4.62
5.00
0.448
0.003
-3.408
0.00
Pre Question
5
4.57
5.00
0.457
0.083
-1.826
0.000
Post Q5
4.71
5.00
0.314
0.083
-1.826
0.00
Pre Question
6
4.48
5.00
0.462
0.042
-2.169
0.000
Post Q6
4.67
5.00
0.333
0.042
-2.169
0.000
Missing
Data
0
Five Wishes
Questionnair
e
Cronbach’s
Alpha
Reliability
0.771
Table 4 Data Definitions
Data Definition Codes
Patient ID Code
Patient Initials and last 2 numbers of MR
number
Age
Age
Gender
1=Female
2= Male
Race(self-identified)
1=White
2=Black/African American
3=Asian
4=Declined
5=Other
Ethnicity(self-identified)
1=Non-Hispanic
2=Hispanic
3=Decline/refuse to answer
4=Other
Question1: Do you have an Advance
Directive?
1=Yes
2=No
3=Missing
Question 2: Do you know what an advance
directive is?
1=Yes
2=No
3=Missing
Question 3: Do you want to discuss Advance
Care planning today?
1=Yes
2=No
3=Missing
Employment Status
1=Employed, Full Time
FIVE WISHES 65
2=Student
3=Retired
4=Self-Employed
5=Missing Data
6=Not Employed
Marital Status
1=Married
2=Single
3=Divorced
4=Widow
5=Missing
Insurance
1=Commercial
2=Medicaid
3=Medicare
4=Self Pay/Uninsured
5=Tricare
Discussion
1=yes
2=no
Provider Engagement
1=Yes (pt wanted discussion) and yes
Discussion took place
2=Yes (wanted) and No discussion took place
3=Not wanted and yes discussion took place
4=Missing response but yes discussion took
place
5=Not wanted/missing data and no discussion
took place
FIVE WISHES SEMINAR PATIENT ID
Initials and date of attendance
Pre/Post Five Wishes Question 1
0=N/A
1=Strongly Disagree
2=Disagree
3=Neutral
4=Agree
5=Strongly Agree
Pre/Post Question 2:
0=N/A
1=Strongly Disagree
2=Disagree
3=Neutral
4=Agree
5=Strongly Agree
Pre/Post Question 3:
0=N/A
1=Strongly Disagree
2=Disagree
3=Neutral
4=Agree
5=Strongly Agree
FIVE WISHES 66
Pre/Post Question 4:
0=N/A
1=Strongly Disagree
2=Disagree
3=Neutral
4=Agree
5=Strongly Agree
Pre/Post Question 5:
0=N/A
1=Strongly Disagree
2=Disagree
3=Neutral
4=Agree
5=Strongly Agree
CPT/ ICD10 claims total (all insurances)
Total number (n)
CPT Reimbursement from billing claims
(Anticipated)
Anticipated Dollar value ($)
CPT Reimbursement (Actual)
Actual Dollar Value ($)
Total number of Discussions 3 months prior
to Intervention at the same office with the
same providers
Total number (n)
Table 5: Variable/Analysis Table
Independent Variable
Dependent Variable
Statistical Analysis
Five Wishes Pre-Seminar
Questionnaire (pre/post, same
patients)
Five Wishes Post Seminar
Questionnaire (pre-post, same
patient)
Paired t test
Total ICD10 EHR
documentation 3 months prior
to intervention at same
practice location, same
providers but different
patients from the same
practice
Total ICD10 EHR
documentation after
Intervention (same practice,
same providers, different
patients from same practice)
Chi Square analysis

FIVE WISHES 67
Dear Amanda and Dr. Ricciardi,
Firstly, in reading your proposal, it is well written and thoughtful. One thing that stood
out to me from an ethical perspective is the choice to exclude persons who are blind.
This exclusion impacts the direct benefit a patient may receive from engaging in the
ACP process. I strongly encourage you to reconsider this exclusion.
Additionally, patients whose first language is not English may also benefit from the ACP
process. Again, I encourage you to seek ways to better include these patients. In
examining the risk/ benefit of the project, these patients may be at greater risk to not be
included in the process as ACP is such a vital component of any holistic care. Also
suggested is the following article that may guide you in engaging these
populations: Hines, S. C., Glover, J. J., Babrow, A. S., Holley, J. L., .Badzek, L. A., &
Moss A.H. (2004). Improving advance care planning by accommodating family
preferences. Journal of Palliative Medicine, 4(4), 481-489.
This all said, regarding the determination worksheet for the project entitled, "Using Five
Wishes to Promote Advance Care Planning in A Maryland Primary Care Practice," a
determination has been made that your project does not meet the definition of research.
That is, a systematic investigation intended to contribute to generalizable knowledge.
This determination is being made after review of the project documents. The project
nature as quality improvement intends to inform internal practice. The project does not
aim to inform new theories or external standards of practice. Therefore, further review
by the GW Nursing Office of Research or the GW Institutional Review Board is not
required (per GW IRB Policy HRP-010, Human Research Protection Program).
Should your project change in any way that it would meet the definition of research,
please contact the GW Nursing Office of Research at [email protected] so we
may assist you in proceeding. As a reminder, you are to conduct all projects in an
ethical manner regardless of review requirements.
Please do not hesitate to contact me with any questions or concerns regarding this
determination.
Kind regards,
Cortni Romaine, PhD Candidate, MS, CIP | Research Program Associate
The George Washington University School of Nursing
Member, GW Institutional Review Board
FIVE WISHES 68
Letter of Cooperation
Dear Sir:
This letter confirms that l, as an authorized representative of Comprehensive Primary Care, allow the PI
access to conduct study related activities at the listed site, as discussed with the PI and briefly outlined
below, and which may commence when the PI provides evidence of IRB approval for the proposed
project.
DNP Project Study Sites: 5413 West Cedar Lane, Suite 203C, Bethesda MD 20814
Study Purpose: To improve education about the advance directive, Five Wishes and
implementation of Advance Care planning
Study Activities: educational assessment, questionnaires, Educational videos
Subject Enrollment: All patients over 18 with an interest in advance care planning and all
voluntary patients who want to learn about Five Wishes.
Site Support: Provide space, authorize site employee's assistance, distribute questionnaires,
allow access to ECW patient records and billing information, allow use of practice equipment,
and identify eligible patient subjects.
Data Management: patient identified information will be protected, vital signs data will be
collected
Anticipated End Date: May 30, 2020
We understand that this site's participation will only take place during the study's active IRB approval
period. All study related activities must cease if IRB approval expires or is suspended. I understand that
any activities involving Personal Private Information or Protected Health Information may require
compliance with HIPAA Laws and GWIJ Policy.
Our Organization agrees to the terms and conditions stated above. If we have any concerns related to
this project, we will contact the Pl. For concerns regarding IRB policy or human subject welfare, we may
also contact the GW IRB.
Regards,
