a
Getting Started
So many of us forget about health insurance until we
need to use it. Even when we have insurance, sometimes
we forget about the routine and preventive services that
help us to get and stay healthy. It isn’t just an expense; it
is a plan. It is also an important decision.
The Nevada Division of Insurance and the Silver State
Health Insurance Exchange are here to help you choose a
plan that is right for you. In the next few pages you will
learn about the different types of health insurance,
when to purchase insurance, important things to look
for, and where to go to complete your purchase.
Nevada Division of Insurance
Talk to us. We're here to help

Why Everyone
Needs Insurance
Many people who feel very healthy, are
active, and practice healthy behaviors, may
think they do not need insurance, especially
due to the cost. Part of staying healthy is
receiving essential routine and preventive
services. Even if you look and feel healthy,
you may not be getting the routine care
you
need to identify the unexpected such
as:
•
Routine lab work used to prevent,
diagnose and control chronic
conditions such as diabetes;
•
Immunizations to avoid illness such as the measles or
•
Cancer screenings that can result in earlier detection
Without insurance, we often avoid thinking about
selecting a primary care physician or developing a plan
for settling hospital bills. Let’s face it, life is full of
surprises. Insurance helps you prepare for the unex-
pected, like your child contracting a common infection
which requires antibiotics such as strep throat, a
do-it-yourself project accident that could require stitches,
or a slip on winter ice. Things like this can happen to
anyone, which is why it is critical to be prepared and
protect yourself and your family. Sometimes having
insurance might motivate us to use it to take better care
of ourselves. Having insurance reduces stress in our
daily lives in knowing we have a plan
for the “what-ifs” of the future. Everyone needs
health insurance.
Even if you already have
insurance, open enrollment is
a great time to update your
insurance and make sure your
current plan is the best plan
for you.
A health plan can be
purchased outside of open enrollment if you
experience certain qualifying life events (QLE), such
as losing coverage from an employer, moving, getting
married, or having a baby. If you do not experience one
of these QLEs, you must wait for the next open
enrollment period to purchase a policy through the
Exchange. Off-Exchange carriers can be found under
the Health Insurance Rates tab at doi.nv.gov.
You can usually only shop for health
insurance
during a specific
period of
time
called
open enrollment.
Cost
of a
up to $7,500
without insurance
Broke
n Leg
Cost
of a
HospitalStay
Source: Healthcare.gov, 2021
1
Without Health Insurance
tetanus; and
and treatment such as a mammogram or prostate exam.
When is the Right Time
to Buy Insurance?
You can usually only
shop for insurance on the Silver State Health
Insurance Exchange
during a specific time frame that
occurs once a year called open enrollment. During
open enrollment, you can purchase a new plan or
change your insurance plan. Open enrollment typically
starts in November and ends in January. You can find
the dates of the next open enrollment on the web at
Nevadahealthlink.com, which is the health insurance
exchange website operated by the Silver State Health
Insurance Exchange, a marketplace where you can buy
insurance. You can also compare options and costs by
visiting http://www.doi.nv.gov.
All health insurance plans provide guaranteed
renewal of coverage, which means that you can stay in
the
plan you have if you like it, and the insurance
company still offers it. The costs of your health
plan
can change from year to year. To see if your costs
are
increasing and look at other options, check
Nevadahealthlink.com
to find out if there’s a better
plan available for you. The Nevada Division of
Insurance (DOI) reviews these plan changes and their
costs every year. If you would like to learn more about
this process or
comment on proposed changes, visit
the DOI website at doi.nv.gov.
What Does Insurance Cover?
Insurance plans help you pay for the things you
need to get healthy and stay healthy, including visits
to
doctors and other pro viders, prescription drugs, and
help during an illness. Any new plan you purchase
covers some or all of the cost of the following basic
items and services, although it is important to know
certain services require prior approval from your
health
plan before you get them. The covered services
are:
•
Hospitalization
• Specific prescription drugs
• Emergency services
•
Outpatient care (care outside of a hospital stay)
•
Preventive services such as immunizations, pap
smears, mammograms, and blood pressure screenings
•
Mental health and substance use disorder services
such as counseling and psychotherapy
•
Wellness services such as disease management
•
Care throughout pregnancy (pre-natal/delivery/
post-natal)
• Basic laboratory services
• Pediatric services
•
Rehabilitative and habilitative services and devices
such as wheelchairs and speech generating devices
•
Contraceptives
•
Pediatric dental and vision care for
children 18 and under
While all
of these items are covered by every
plan, there are differences in how plans
cover the costs of these items. You can learn
about these on the next page of this guide.
Some plans may also offer
additional
s services such as adult dental and vision
care,
family planning services, cancer screening and
more.
Regardless of which plan you choose, the Affordable
Care Act requires that all preventive health services are
made available to consumers at no cost. You should
not
be charged for these services.
The Affordable Care Act requires
that all preventive health care
services are made available to
consumers
at no cost.
2

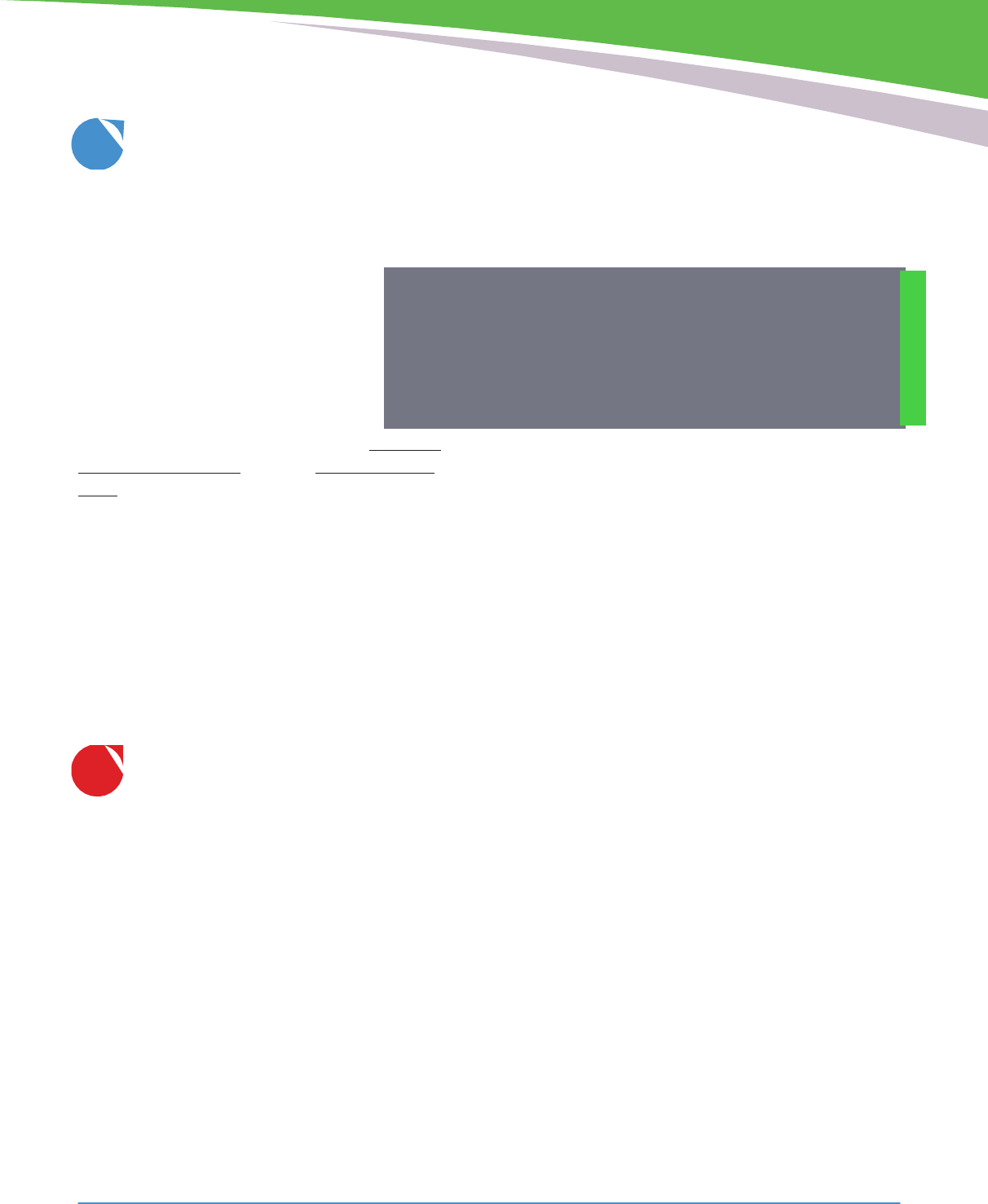
Primary Care Providers
Sometimes the way you access different kinds of
doctors
and other providers can vary by what type
of insurance plan you have. Understanding how the
different models work is a good way to start thinking
about which plan is right for you.
For example, some insurance plans require you to see
your primary care physician and obtain a referral in
order to see a doctor for specialized services. It is your
responsibility to select a
primary care provider
(PCP).
Examples of these models are a Health
Maintenance Organization or
HMO
or Exclusive
Maintenance Organization or EPO. These models
focus on ensuring
that a healthcare provider is
managing all of your care through a single point of
coordination, your PCP.
Other insurance models allow you to see certain doc-
tors, providers, or specialists at any time. One example
of this model is a Preferred Provider Organization or
PPO.
PPOs focus on direct access to providers that
are
part of the insurance plan or network. While you
should
always have a PCP, if you have a PPO you will
not need
your PCP’s approval to see other types of
providers.
However, some services, such as a CAT scan or certain
procedures, may still require special authorization.
Consider how often
you visit a
doctor. Do you see your PCP or
specialists more often? Your
answer can help you decide if
a PPO or HMO is better for
your needs.
PREFERRED PROVIDER
How Do I Know
Which Plan to Choose?
There are three main questions to ask that will help you
narrow the search for the right plan:
Do you need access to a specific doctor or
other care provider?
The doctors and other caregivers a plan works
with is called the
plan provider network.
You will
pay less to see providers that accept the health insur-
ance plan you buy. This is called
in-network.
You
will pay more to see providers that do not accept
your health insurance plan. This is called
out-of-
network.
Each insurance company publishes a
list of the providers available in their plan on their
website. That list is called a
provider directory.
If
you like the doctor you have, you can ask your doctor
HEALTH MAINTENANCE
ORGANIZATION
HMO
ORGANIZATION
PPO
which insurance plans they accept or you can check
these directories at any time to see if your doctor is
in-network.
Some plans have more providers in their networks
than others. Plans with more doctors tend to cost more
while plans with fewer doctors cost less. Think about
how much you want to pay and how much you
value options for the providers you see when deciding
whether a plan’s network is right for you.
1
3
EPO
EXCLUSIVE PROVIDER
ORGANIZATION
Do you need a specific medical service or
prescription drug?
If you need a special type of medical service or
take
a specific prescription drug, you can also check
that the service or drug is covered under the insur-
ance plan you are considering. You can
see if a medical service is covered by
reading the plan’s
Schedule of
Benefits
(SOB), which is a
short, easy-
to-understand summary of
a plan’s
benefits and coverage. Every plan offers
an SOB when
you're shopping,
and you’ll find a link to each plan’s SOB
at
doi.nv.gov.
This is located by clicking Search for
Health Insurance Rates under the Health Insurance
Rates tab. Instructions on how to find the plan's
SOB, Evidence of Coverage and carrier Contact
Information is also located under the Health
Insurance Rates tab.
The list of drugs covered under an insurance plan is
called a
formulary.
Like the provider directory, plan
formularies are available online. Plans often
categorize
drugs in terms of preferred or non-
preferred. If a drug
is preferred, it may mean that the
fee paid when you fill
the prescription is lower.
What mix of costs and fees work best
for you?
Let’s look at the different costs you will pay for your
health insurance.
Monthly Premiums
When you buy insurance, the monthly bill from your
insurance company is called a
premium.
Sometimes a
premium is called the sticker price, like when you buy
a car, because it’s the first price you see, but it is not the
total cost of your healthcare.
Insurance companies set a base rate for everyone who
buys a health insurance plan and then adjust that rate
based on just a few things: the number of people in
your family you are shopping for, age, location, and
tobacco use. The final calculation to the rate as it
applies to you, taking those factors into consideration,
becomes your fixed rate, or monthly premium.
Insurance companies can no longer charge you a
higher premium based on your health status or due to
pre-existing medical conditions.
We know that premiums are up-front monthly costs.
The other costs – copays, deductibles, coinsurance, and
Insurance companies can no longer
charge you a higher premium
based
upon your health status
.
out-of-pocket limits – are costs paid when you receive
care. Generally there is a trade-off in monthly costs
and
the costs you pay when you receive care. The
higher the
monthly premiums, the lower your costs will
be when you
receive care.
Copays
Fees charged at the time you receive service, whether
a trip to the doctor or picking up a prescription at the
pharmacy, are called
copays.
Copays can be different
depending on the type of service you receive. For
instance, a copay to your in-network doctor might be
$20. A copay for a specialist might be $45. A copay to
your pharmacy might be $5 for a preferred drug versus
$10 for a non-preferred drug.
Deductibles
A
deductible
is the amount you need to pay first
before your insurance company will begin to cover
the cost of your care. Premiums and copays usually
don’t count toward your deductible. Also, deductibles
do not apply to all services. Most plans cover routine
visits, necessary prescription drugs, and preventive
care outside of your deductible. Once you’ve met
your
deductible, you and your insurance company share
the cost of your care until you’ve met your
out-of-
pocket limit.
Coinsurance
Coinsurance
is similar to a copay. It is a charge due at
the time of a specific (and usually less routine) service,
such as hospitalization, but as a percentage of the cost
of that service instead of a fixed fee.
3
4
2
Out-of-Pocket Limit
The
out-of-pocket limit
is the most you
will have to pay each year for covered
services outside of your monthly bill/pre-
mium. The federal government tells health
insurance companies how high they can
set the out-of-pocket limits. In 2022, the
out-of-pocket limit for an individual could
be no more than $8,700 and no more than
$17,400 for a family, although many
plans offer out-of-pocket limits lower than
these. Once you reach the out-of-pocket
maximum, insurance pays for 100% of your medical
care (for in-network covered services only), although
you will continue to pay your monthly premium. Out
of network services are covered differently and often
result in significantly higher out-of-pocket costs. Check
to see how your plan covers these services before
seeking care from an out-of-network provider.
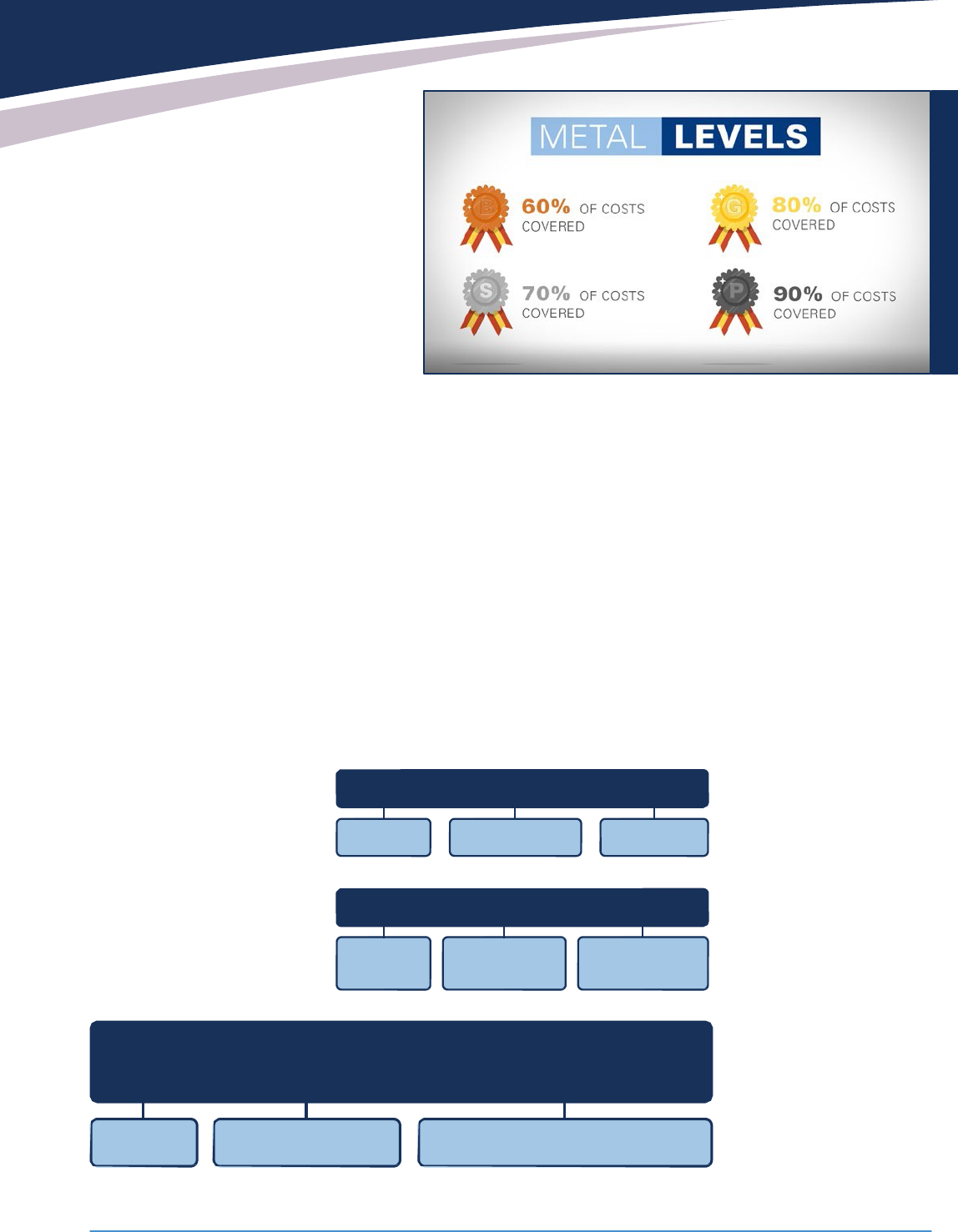
Balancing Costs
How do these costs fit together? The illustrations below
are examples that may help you understand these costs.
Keeping Track
Your insurance plan keeps
track of your costs. Each time
you use your insurance, your
insurance company sends
you a statement that tells you
how you used your benefits. It
is like a receipt. This is called
an
Explanation of Bene-
fits (EOB). An EOB will tell
you how much your provider
charges, how much the insurance plan will cover, and
how much you are responsible for/owe your provider. It
will also tell you how far along you are in meeting your
deductible and out of pocket limit. If you are asked to
pay for costs, other than your monthly premium, once
you’ve reached your out-of-pocket limit, you should
contact your insurance company.
Remember there is a trade-off between monthly costs
and the
costs you pay when you receive care. That
means that
generally insurance plans with low
premiums have
high deductibles and out of pocket
limits, and vice-versa. Once you find the balance in
costs that you think
is best for you, it can be easier to
select a plan using a
system called metal levels.
You can stop paying copays, deductibles and coinsurance once your out-of-pocket limit is met.
Each metal level, (shown in
the chart above), represents
the percentage of costs you
and your health plan
share,
outside of your
premium,
based on an
average. For
instance,
someone with a
bronze
level plan can
expect to pay 40% of their
health-
care cost on
average each
year, silver
30%, gold 20%, and
platinum 10%, with
the
health insurance plan
covering the rest.
Depending on how you use
your
insurance and the
amount
of monthly costs
you can
afford, one of these
options
may be a better fit.
Out-of-Pocket Costs Include
Copays
Coinsurance
Deductibles
Out-of-Pocket Costs Don’t Include
Premiums
Non-covered
Out-of-Network
Services
Charges
OUT-OF-POCKET LIMIT
=
DEDUCTIBLE
+
COINSURANCE
+
COPAYMENT
If the Out-of-Pocket limit is met, you must only pay:
Premiums
Non-covered Services
Out-of-Network Charges & Balances
5
Can I Get Help Paying
for Insurance?
There are several ways in which you may qualify for
assistance to help lower your health care costs. The
Affordable Care Act includes two ways for you to
reduce your costs called
subsidies.
The first subsidy
reduces your premium and is called the
Advanced
Premium Tax Credit (APTC).
The APTC is based on
family size, the estimated household income for
the
coming year, and the average price of insurance
plans. If you qualify for an APTC, you may choose to
receive the subsidy as a tax credit, or send the infor-
mation about your subsidy directly to your health
plan through the Exchange, where they will apply it
to your monthly premium as a credit lowering your
monthly premium. You will receive a 1095 form to
file
with your annual tax return from the Health
Insurance Exchange to reconcile your income if you
qualify for an APTC. This form must be filed to ensure
your qualifications and credits are accurate. This may
also result in owed taxes or an additional
refund or
credit if your income was higher
or lower than expected for the year.
The second subsidy is called a
Cost-Sharing
Reduction (CSR).
Individuals and families
whose household income falls between
138%-250% of the Federal Poverty Level
are eligible for cost-sharing reductions (or
CSRs) if they are eligible for a premium tax
credit and purchase a silver plan through
the Exchange. People
eligible for cost-
sharing reductions will
automatically receive
a version of the plan
with reduced cost-
sharing charges,
such as lower deductibles, out-of-
pocket
maximums or copayments.
Unlike the premium subsidies, cost-sharing reductions
are not provided as a tax credit and they do not have
to
be “reconciled” when people file their taxes for the
year
the cost-sharing reductions were received.
Many people who think they don’t qualify for a
subsidy actually do. For example, a family of four
with an income level of $100,000 in 2022 qualifies
for a subsidy to lower their premium. The only way
to receive a subsidy is to purchase your
insurance through the marketplace
on
Nevadahealthlink.com
.
Depending on your circumstances or
income level, you may also qualify
for
other assistance such as the
Federal
Medicare Program, Medicaid (Medical Assistance
or MA) or the
Children’s Health Insurance
Program (CHIP).
If you qualify,
Nevadahealthlink.com will provide you with more
information
on the programs that are offered by the
State of Nevada.
Where to Buy Insurance
in
Nevada
Now that you know all about what to look for
when you are choosing your plan, let’s talk about
where you can go to buy health insurance.
Doi.nv.gov
is a great place to compare multiple
plans
and options
, and find health insurance policies not
available through the Exchange for families that do not
qualify for subsidies.
Many people who think they don’t
qualify for a subsidy
actuall
y do.
6
an enrollment professional. You can find a list to contact
enrollment professionals
in your area directly on
Nevadahealthlink.com. You can also complete your
purchase
by logging into your account on
NevadaHealthLink.com.
Please be cautious if unexpectedly solicited
for health
insurance. As in all other industries, this can be an
opportunity for fraud. Do not supply any financial
or private information until you are sure of the
organization’s
credential
s. You can verify if they are
licensed at doi.nv.gov.
Web
. . . . . . . . . . . . . . . . . . . . . .
www.nevadahe
althlink.com
Email
. . . . . . . . . . . . . .
Phone
. . . . . . . . . . . . . . . . . . . . . . . . . . .
1-855-7NVLINK (855-768-5465)
Web
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
www .doi.nv .gov
Phone
. . . . . . . . . . . . . ..
(888) 872-3234
toll-free or (775) 687-0700
Web
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
www .medicare .gov
Phone
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
1-800-MEDICARE
Nevada Medical Assistance (Medicaid)
Web
. . . . . . . . . . . . . . . . . . . . .
https://dwss.nv.gov/Contact/Welfare/
Phone
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
(877) 543-7669
Web
. . . . . . . . . . . . . . . . . .
https://dwss.nv.gov/Medical/NCUMAIN/
Phone
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
(877) 543-7669
Additional Resources
To check your options, buy insurance,
or get help find
coverage, visit:
Nevadahealthlink.com is the site where you can get
information regarding eligible subsidies to help you and
your family pay for your individual health insurance.
Nevadahealthlink.com can also connect you with
licensed
enrollment professionals
who
are certified
and trained by Nevada Health Link.
These insurance
professionals will help you apply, enroll, and answer
your questions. These professionals are available to
provide face-to-face assistance, that is free of charge.
Nevadahealthlink.com consumer assistance call center
is ready to answer questions
and assist you in finding
Buyer’s Checklist
Now
that you know why insurance is important,
when
to look for a plan, basic items and services
included
in a plan, important things to consider, and
where
to purchase a plan, you are ready to shop!
This
checklist may help you review and prepare for
your
purchase
.
Make sure the providers and services
important to you are available in the plan
you are considering
.
Review your monthly and annual budget to
determine your price range and the right
combination of costs
.
You can use metal levels
as a guide
.
Consider shopping through the Nevada's Health
Insurance Exchange
.
You may be surprised to find
that
you qualify for a subsidy to lower your costs
.
Make sure you have continuous coverage and
always renew or purchase your insurance
during open enrollment
.
Happy Shopping!
7
Nevada Check Up (CHIP)
low-cost, comprehensive health care coverage to low income,
uninsured children (birth through 18)
The Nevada Division of Insurance is very grateful to the
Pennsylvania Department of Insurance for granting us
the use of their content in this guide
